Patients today have more data than ever — labs, wearables, diets, even GLP-1 prescriptions. Yet many still feel stuck. They’re eating better, exercising more, and possibly trying supplements or medications, yet progress still stalls.
As practitioners, we see the frustration — and we share it. Too often, care plans feel like guesswork.
After 25 years in practice, I’ve found the missing piece: a comprehensive Weight-Health Hormone Assessment. Not just another lab result or data point, but a structured way to connect the dots between hormones, metabolism, and lifestyle choices.
Why Current Models Fall Short – It’s Not Lack of Data or Effort
Our patients today arrive with plenty of numbers. But more data doesn’t always equal more insights.
- Labs provide values, but without context — or when they’re not the right labs — they may mislead or fail to explain why symptoms persist.
- Scales showing total body weight (or even body composition) often provide incomplete or poor-quality data.
- Wearables track outputs like sleep, steps, macros, and heart rate. Without context about why choices are made or how the body is responding, these numbers can distract from what matters most.
These tools aren’t bad. But on their own, they leave patients chasing isolated fixes. What’s missing is the bigger picture of how weight-health hormones are functioning, what drives that function, and which interventions will improve outcomes.
Why a Weight-Health Hormone Assessment is Key for Every Patient
For optimal health, weight-health hormones— including GLP-1, GIP, PYY, and CCK — need to function as intended. When they do, they help regulate:
- Bone, muscle, and fat mass
- Blood sugar control
- Appetite and hunger signals
The scale, labs, or digestive assessments each offer partial insights. But when combined in a structured ecosystem — with reassessment built in — we gain a feedback loop that supports experimentation and optimization.
This is the role of the Weight-Health Hormone Assessment: it doesn’t replace other tools. It helps us:
- Determine whether hormone function is optimal or impaired
- Identify what’s driving that function — nutrition, sleep, stress, medications, or digestion
- Create a feedback loop through reassessment that supports experimentation and long-term optimization
Watch this short video where I explain why I created the Weight-Health Hormone Assessment and how it helps us as practitioners.
How the Weight-Health Hormone Assessment Supports GLP-1 Agonist Use (and Discontinuation)
The surge in GLP-1 prescriptions has created new challenges in practice. Patients come in either already on these medications, considering them, or struggling with side effects and stalled results.
The Weight-Health Hormone Assessment helps us:
- Before starting: Evaluate baseline hormone function to set expectations.
- During use: Personalize plans to optimize results and minimize side effects.
- For Discontinuation: Identify where hormone signals need reinforcement to reduce rebound risk.
This shifts the conversation from “medication or no medication” to “How do we optimize your body’s signals so your plan works either way?”
Case Studies: How Practitioners Use the Assessment
- The fatigued “perfect” patient: One patient tracked every bite, exercised daily, and “hit” her macros. Her weight-health assessment revealed sluggish GLP-1 signaling tied to poor sleep hygiene. Adjusting her recovery routines unlocked progress.
- The GLP-1 plateau: A patient on semaglutide initially lost weight but then stalled. The Weight-Health Hormone Assessment revealed suppressed signaling and poor protein timing . With targeted nutrition adjustments, his progress restarted — with fewer GI issues.
- The risk of weight regain: A long-time GLP-1 user wanted to discontinue but feared rebound effects. The Weight-Health Hormone Assessment identified suppressed function and suboptimal protein timing. By addressing both, the patient transitioned off medication and maintained their weight health.
In each case, the assessment didn’t replace labs or medications — it integrated them into a framework that made sense for both the practitioner and the patient.
Moving Beyond “Good Enough”
Patients don’t need more noise — they need clarity. As clinicians, we can provide that clarity.
The Weight-Health Hormone Assessment gives us a way to simplify complex data, empower patients with insight, and improve outcomes through ongoing feedback and optimization.
It’s not about more data. It’s about finding the missing piece that helps everything else fall into place.
Explore Practitioner Resources
With the Weight-Health Hormone Assessment, you’ll have:
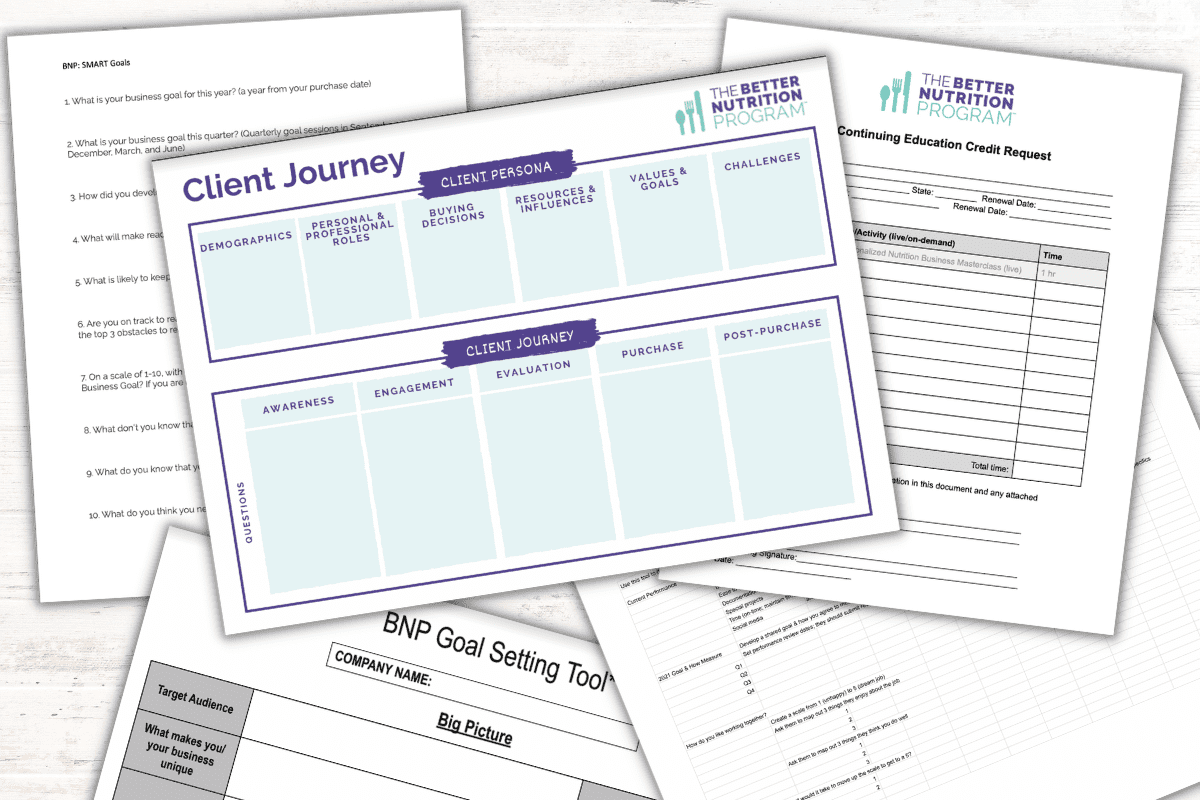
- A structured 3-step framework to evaluate weight-health hormone function.
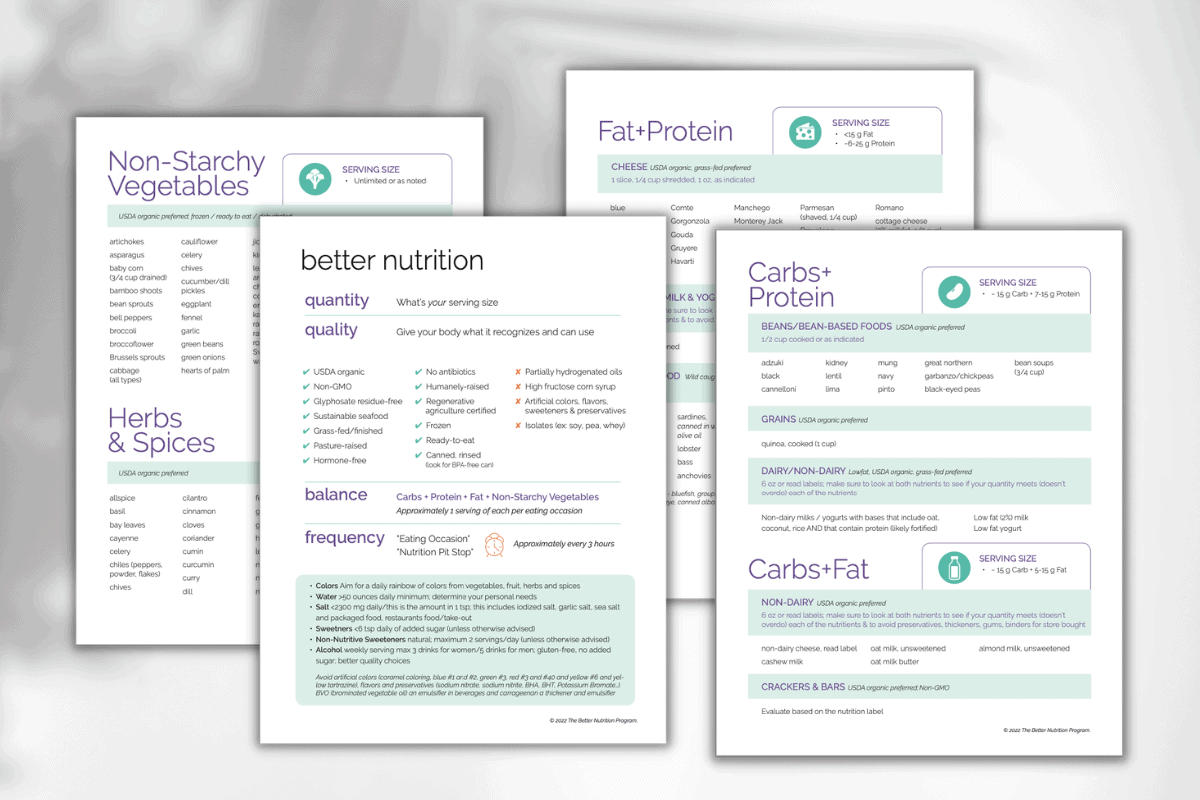
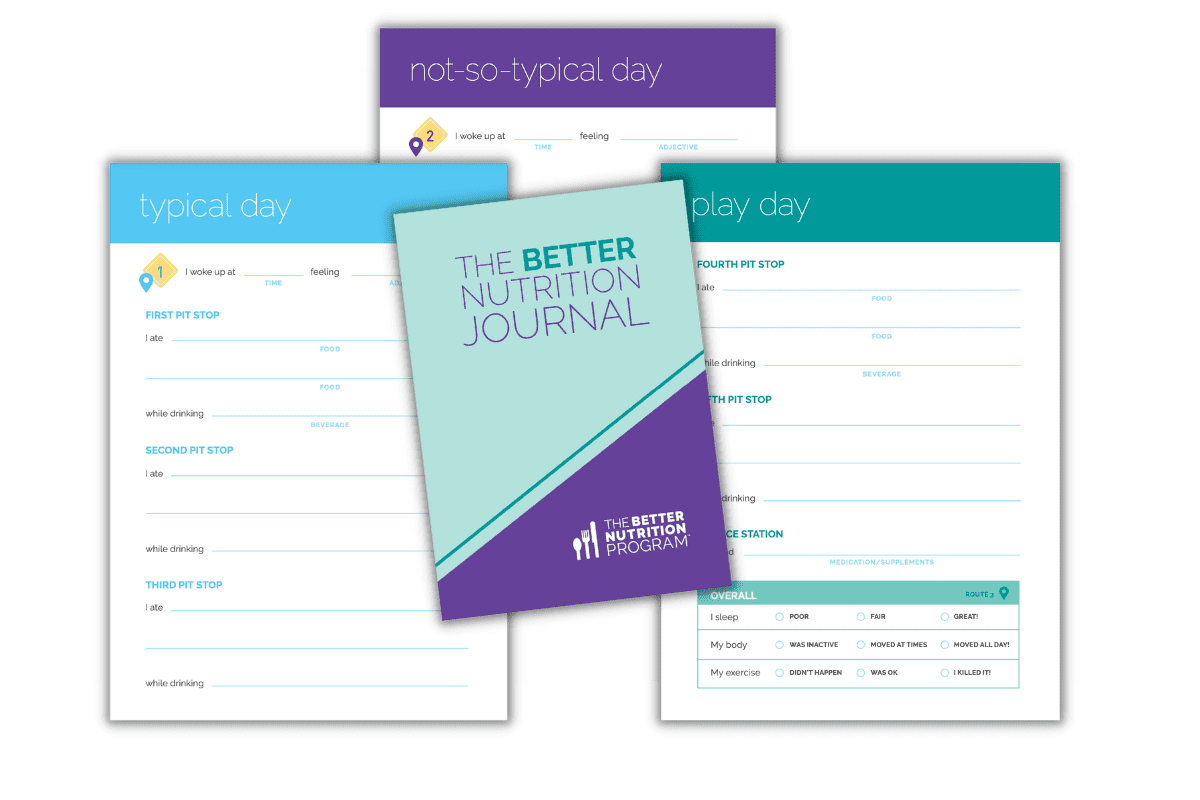
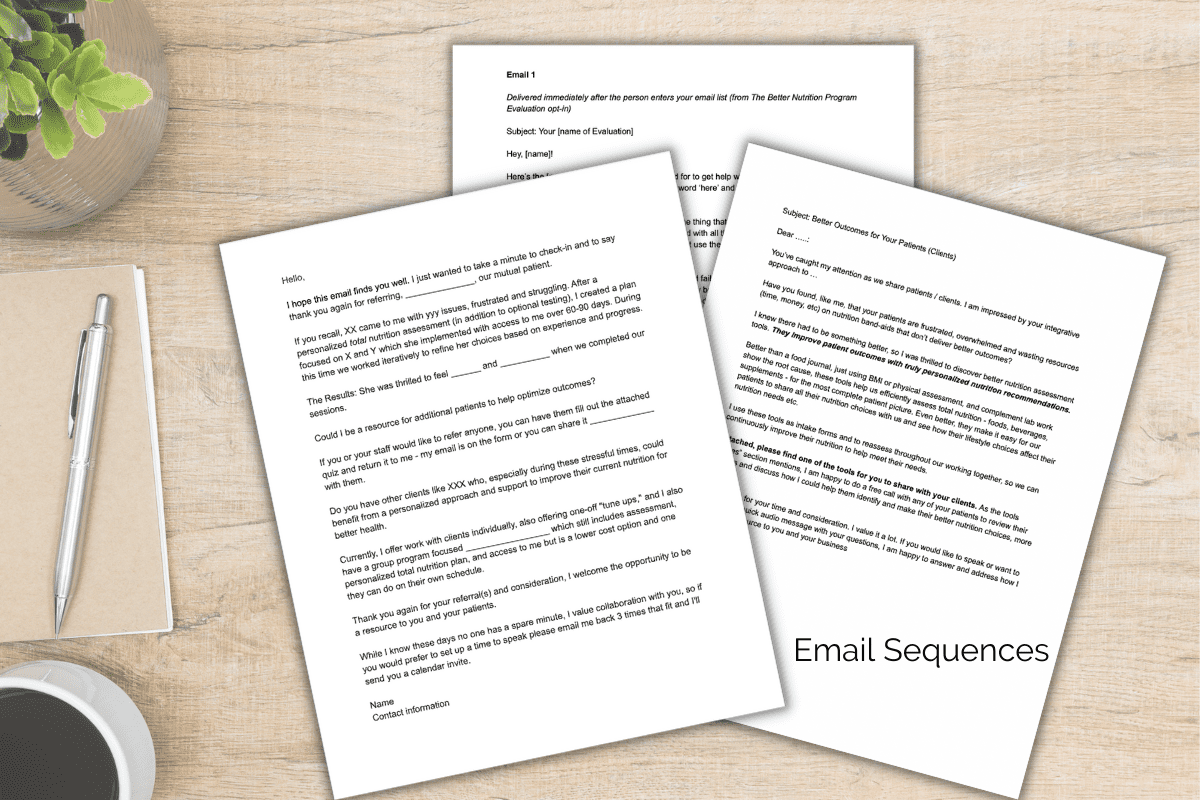
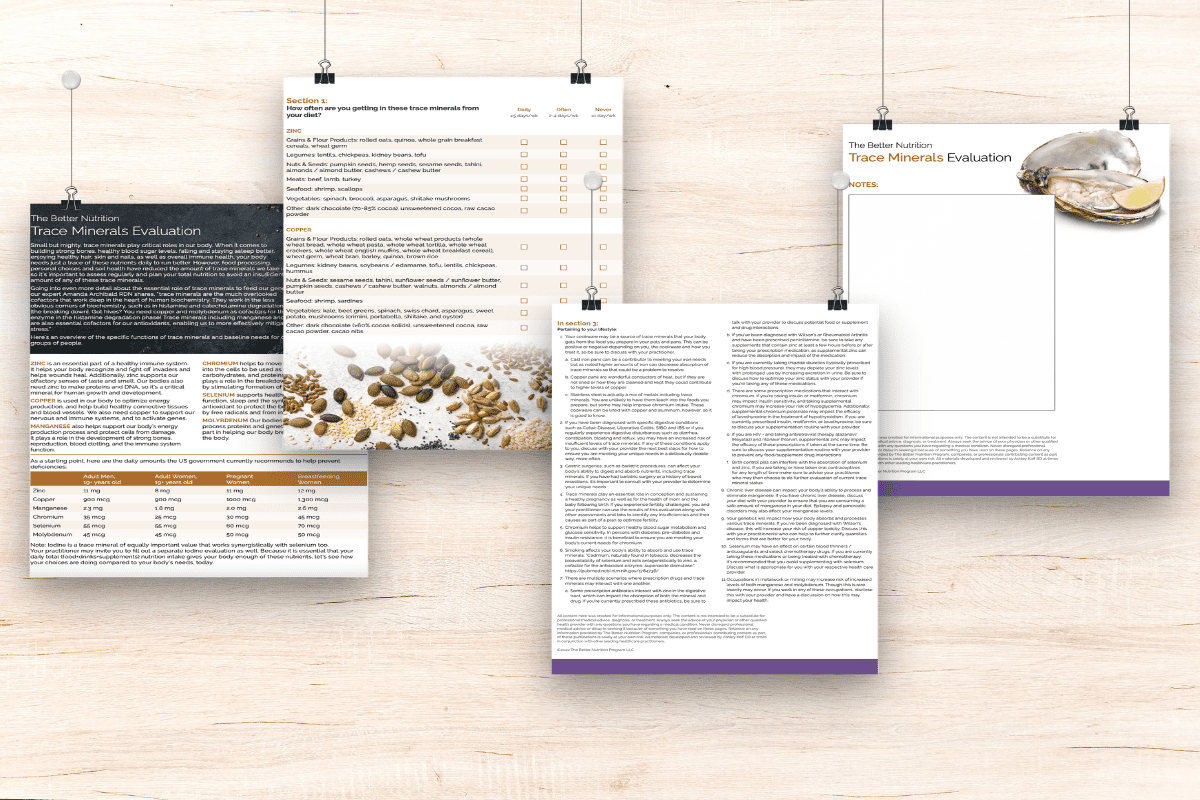
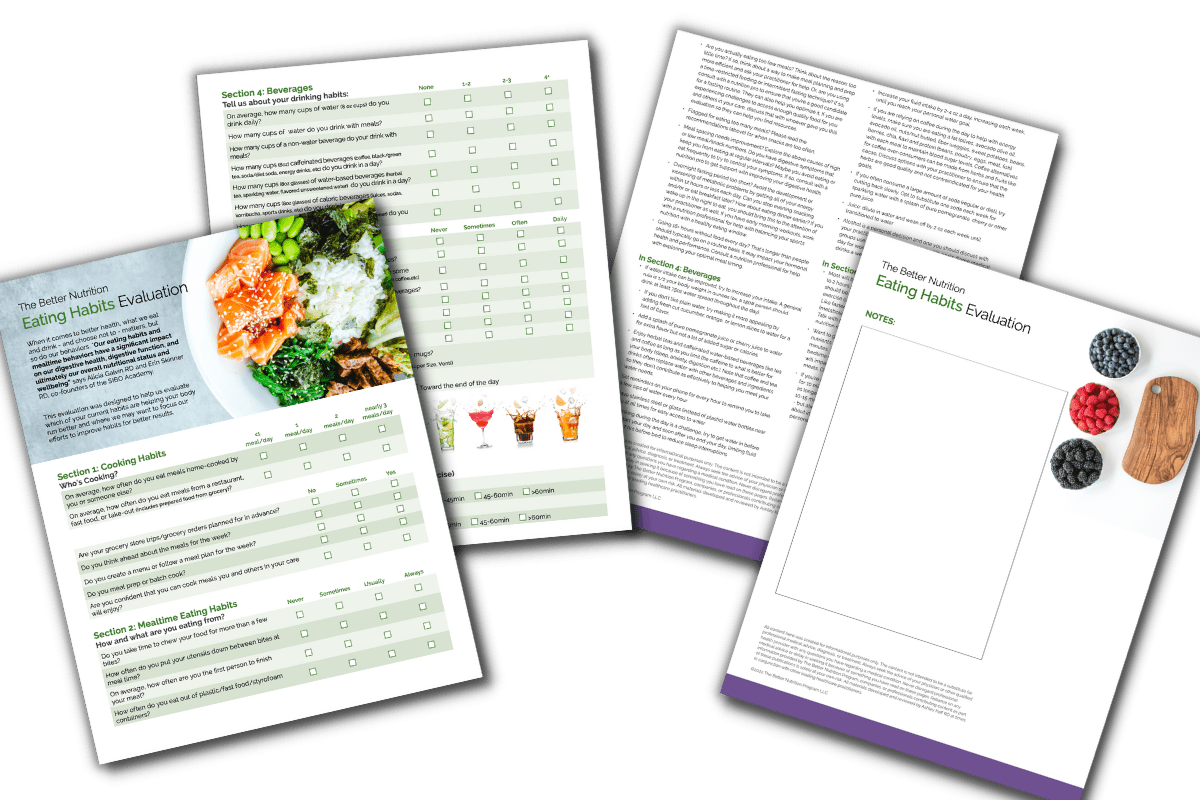
- Patient-ready worksheets and tools that streamline the information-gathering process.
- More explicit conversations — patients arrive with more context, saving you time in consults.
- Integration support for patients on GLP-1s, seeking to start or considering discontinuation of their treatment.
This isn’t about adding more to your plate. It’s about simplifying what you already do — and helping your patients finally connect the dots.
Ready to Get Started?
Integrate the Weight-Health Hormone Assessment into your practice by testing it out yourself first.
Whether you’re supporting patients who are considering GLP-1 therapy, currently on it, or doing “everything right” without results, the Weight-Health Hormone Assessment can help identify the missing piece.
Let’s make weight health more personalized, more practical, and more effective — together.