A growing number of people are using continuous glucose monitors in an effort to personalize their nutrition choices. They want to track what the food they eat is doing to their blood sugar in real time—even those who don’t have type 2 diabetes. Here’s what you need to know to help your clients make the most of their data, plus how to use to truly personalize nutrition recommendations for better outcomes.
In this article, you’ll …
- Understand how continuous glucose monitors work, and why they can be helpful for many clients
- Learn how to use clients’ continuous glucose monitor results to personalize nutrition recommendations
- Identify a toolkit you need to have better conversations with your clients about eating for optimal blood sugar
- Recognize which clients might benefit the most from using a continuous glucose monitor, and learn about the various options on the market right now
Scroll through Instagram these days and there’s a good chance you’ll find ads for companies offering continuous glucose monitors (CGM). These medical devices revolutionized diabetes care when they first hit the market back in 2005, replacing finger-prick blood tests with an easier, faster way to measure blood glucose.
This game-changing technology has gotten even better. Big improvements in glucose sensor accuracy, even smaller sensor size, and integrations with smart phone apps. The result? Continuous glucose monitors are better than ever, and are now marketed to all of us—not just diabetics—as a way to better understand how our bodies respond to the food we eat.
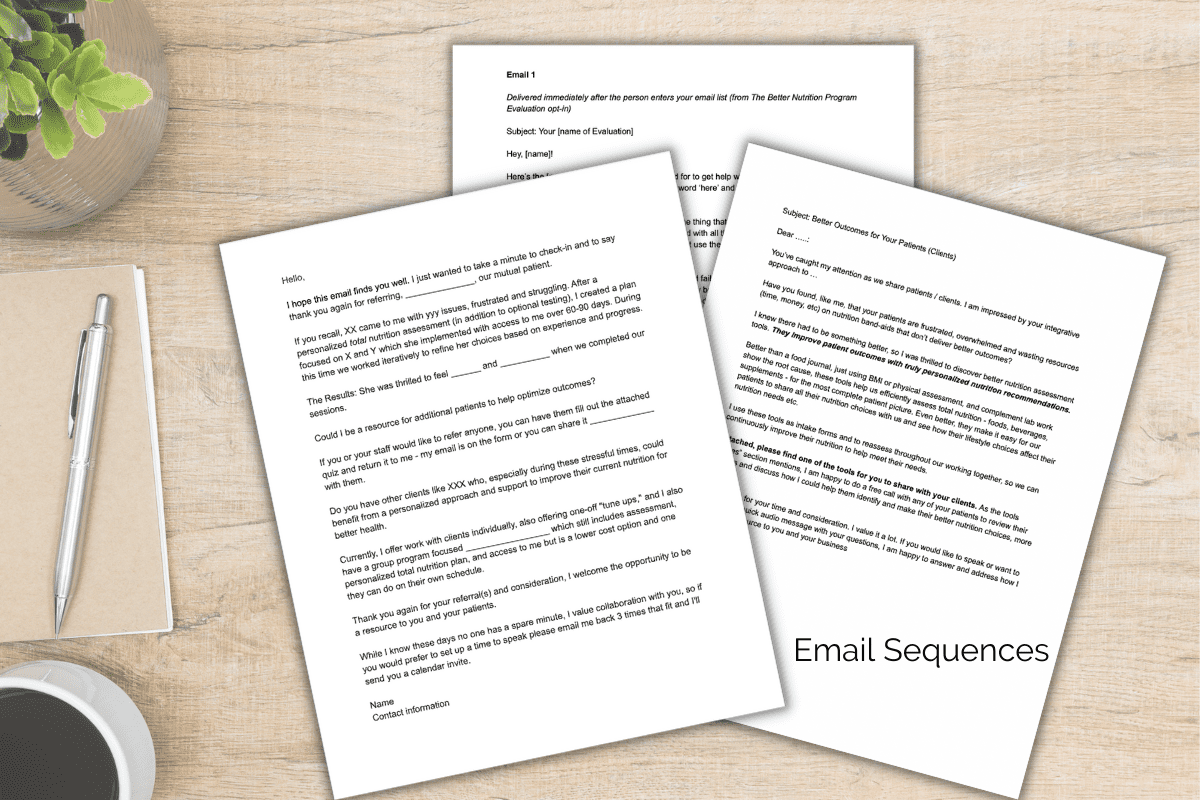
Growing popularity in the use of CGMs means your current clients will likely be coming to interpret the data from their CGM trial. Or your prospects will decide to invest in a CGM instead of working with you. Read on to discover essential information to help you use their CGM readouts to better personalize recommendations and to show prospects why working with you and their CGM is better than going it alone.
First, What Exactly is a Continuous Glucose Monitor—and How Do They Work?
As the name implies, a CGM is a wearable device that attaches to your skin (usually your upper arm) to continuously track glucose levels. Once the CGM is on, the tiny filament in the device monitors and transmits up-to-the-minute glucose levels. The levels are monitored on an accompanying app. The user simply waves their phone over the sensor to transmit blood glucose data for a consistent stream of readouts. After two weeks, most CGMs need to be replaced.
For patients living with type 2 diabetes, CGMs have been a game changer when it comes to monitoring blood glucose. In the not-so-distant past, the only way to monitor blood sugar was by using a lancet device to get a drop of blood from a finger, that was then placed on a test strip for results. Constant finger pricks can be painful, and a nuisance. Thanks to CGMs, managing diabetes is simpler than ever, and being able to see blood glucose in real time helps patients see much more clearly how their body is responding to all the foods they eat.
“CGMs are a wonderful part of a practitioner’s toolkit to show our clients how their choices – food, beverage, supplements, activity, sleep etc – actually impact their blood glucose,” says Ashley Koff, RD, CEO of The Better Nutrition Program. “For example, your client might know that macro nutrient balance is important—but when they see what happens to their blood sugar after eating oatmeal topped with nuts and seeds versus fruit and maple syrup, it’s incredibly motivating.” Similarly, when clients see how a lack of sleep or lots of stress can mess with their blood glucose levels, it can inspire better choices.
Which Patients Benefit Most from Using a Continuous Glucose Monitor?
While CGMs can provide powerful, personalized health information for everyone, there are a number of instances where they are especially helpful—and sometimes even crucial.
- Patients with type 2 diabetes: For those living with type 2 diabetes, a CGM is often a critical component of managing the condition. Sure we can teach carbohydrate counting or advise that some forms are better than others. But seeing what’s happening with blood glucose immediately after eating (in real time!) is even better! Patients can make adjustments right away and avoid extreme swings in glucose that can be dangerous. Even better, a CGM’s accompanying app will alert patients if they’re entering a too-high or too-low danger zone, making managing this disease easier than ever before.
- Patients with prediabetes: For patients diagnosed with prediabetes, knowing how choices and quantity affect their personal blood sugar levels can prove challenging. While many doctors advise patients to simply reduce sugar and exercise more, knowing what types of food and exercise —plus how much and when—can feel like the ultimate guessing game. Enter a CGM, which can show your clients how their everyday choices directly impact their blood glucose levels for better and worse in real time. To wit: One recent study found that CGMs helped adults with prediabetes make better diet choices because the monitor helped them visualize the effect specific carbohydrates had on their blood sugar.
- Patients with insulin resistance: For patients with impaired glucose control who don’t have diabetes or prediabetes—such as women with polycystic ovary syndrome (PCOS), those in menopause, as well as smokers or those with excess belly fat—a CGM can be a helpful tool to make their better choices for more effective blood sugar management.
- Patients who want to improve their overall health: For patients with normal blood glucose levels looking to personalize their diet and optimize their health, a CGM can be a great tool—and can often be used for a short period of time, rather than for continued maintenance. Using a CGM for even just one month can provide a detailed look at someone’s metabolic and nutritional health. It can go a long way toward helping understand what foods work optimally for better blood sugar management, a cornerstone of better health.
3 Steps to Personalize Nutrition Recommendations with Continuous Glucose Monitor Results
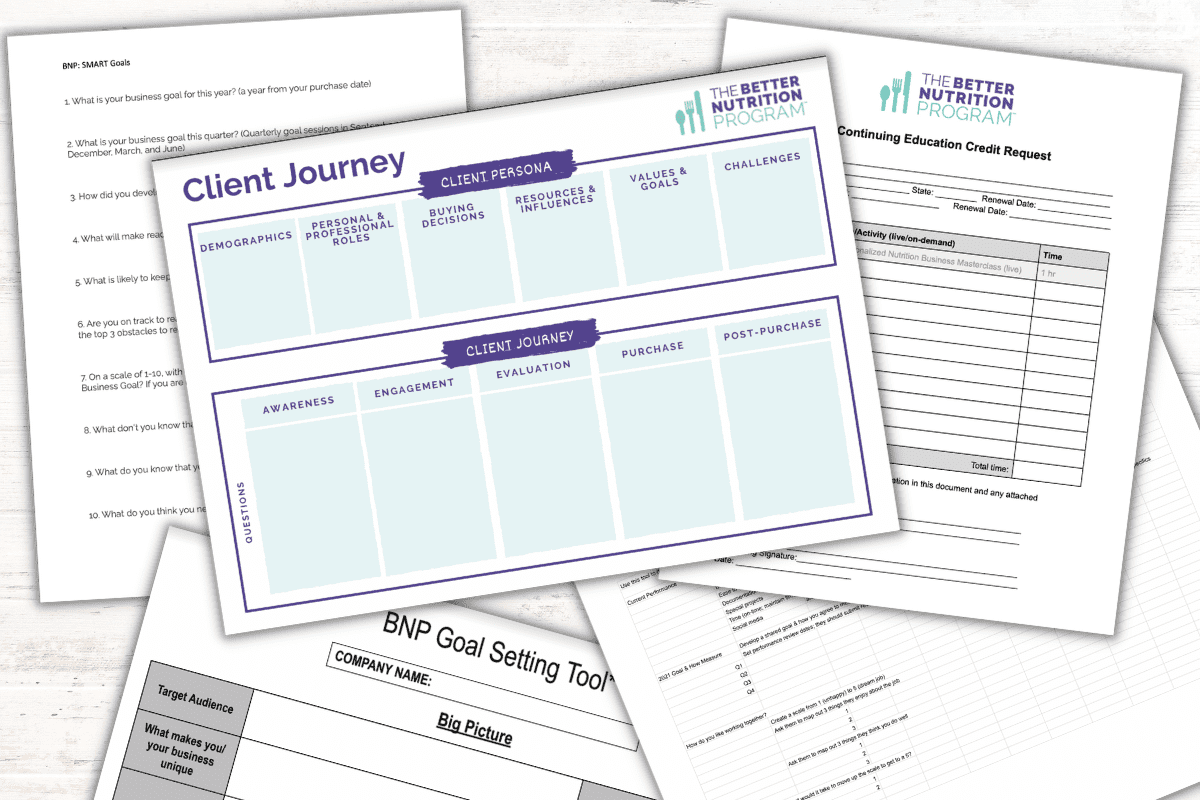
Working with you helps any individual upgrade their CGM results powered by personalized nutrition recommendations. When you take them through these steps you differentiate yourself and show them what they need to truly optimize their results.
Step No. 1: Understand your clients’ “why.”
If one of your clients shares with you that they’re using a continuous glucose monitor, getting a sense of their motivation for using the device will help inform the nutrition strategy you create. For example, is your client in the prediabetic range and using the CGM to see which foods may be causing her elevated blood sugar? Or, was your client lured by an Instagram ad or magazine article, and invested in a month-long CGM experience to gain more insights about how her body is responding to the food she’s eating and what changes she can make to lose weight? While the reasons your clients will use a CGM will vary, understanding their “why?” is an essential first step to devise a plan that’ll help each client make the most of using a CGM, says Koff.
Step No. 2: Evaluate your clients’ digestion.
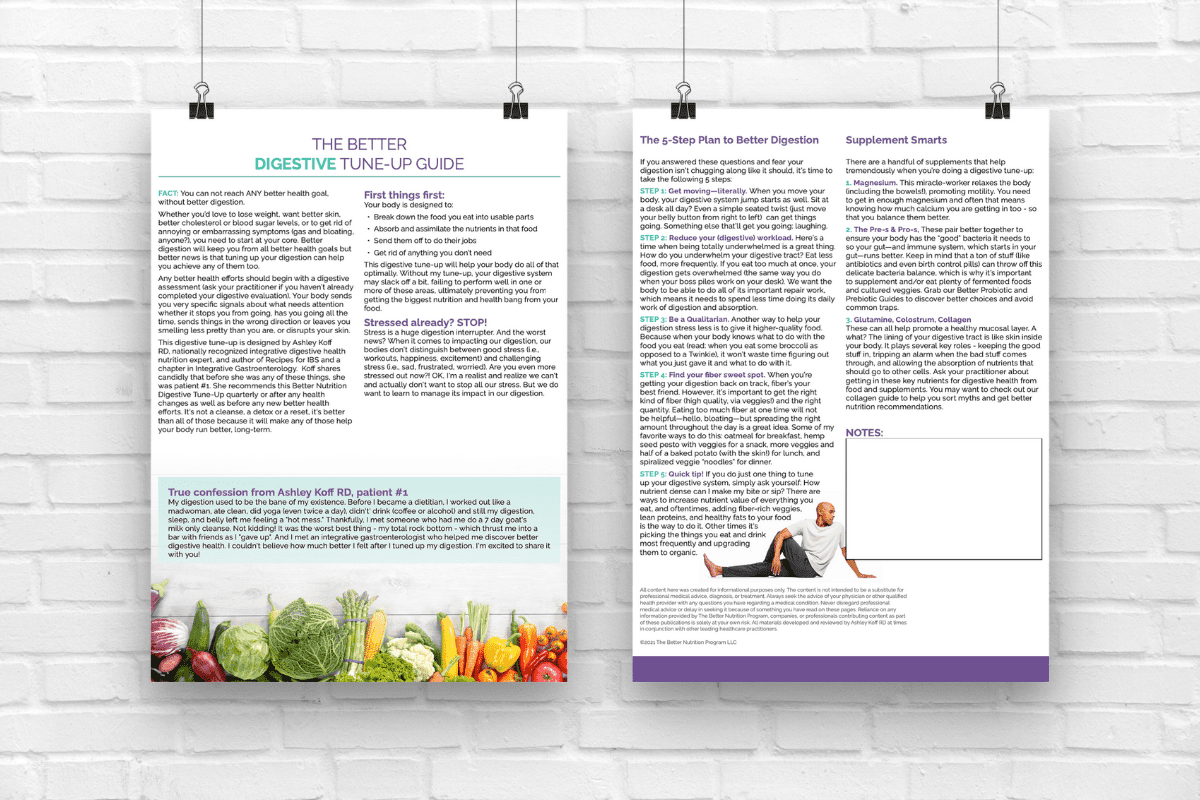
Just as important as understanding why your clients are using a CGM is getting a sense of their digestive health, says Koff. She says she uses the BNP Digestive Evaluation before a patient uses a CGM, and often repeats the evaluation four to six weeks after beginning the CGM and making any adjustments. She may also review additional labs and tests that help her assess their current digestion. “While a CGM will give you a sense of how specific foods are impacting your blood sugar, it won’t give you insights into digestive health which is essential to understand how their body is able to get and use nutrients” says Koff. For example, if a client has an irritated digestive system, that will impact blood sugar levels and should be addressed before changing foods and quantities.
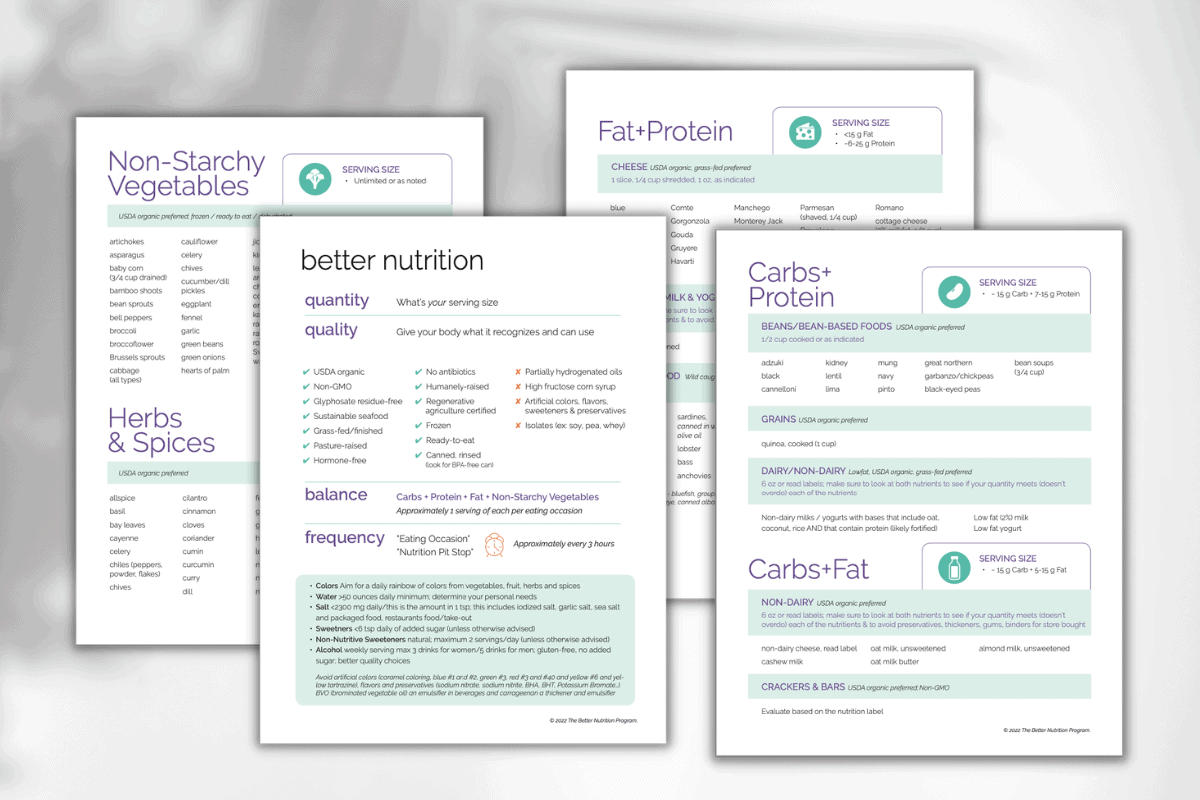
Step No. 3: Personalize to Meet Their Needs
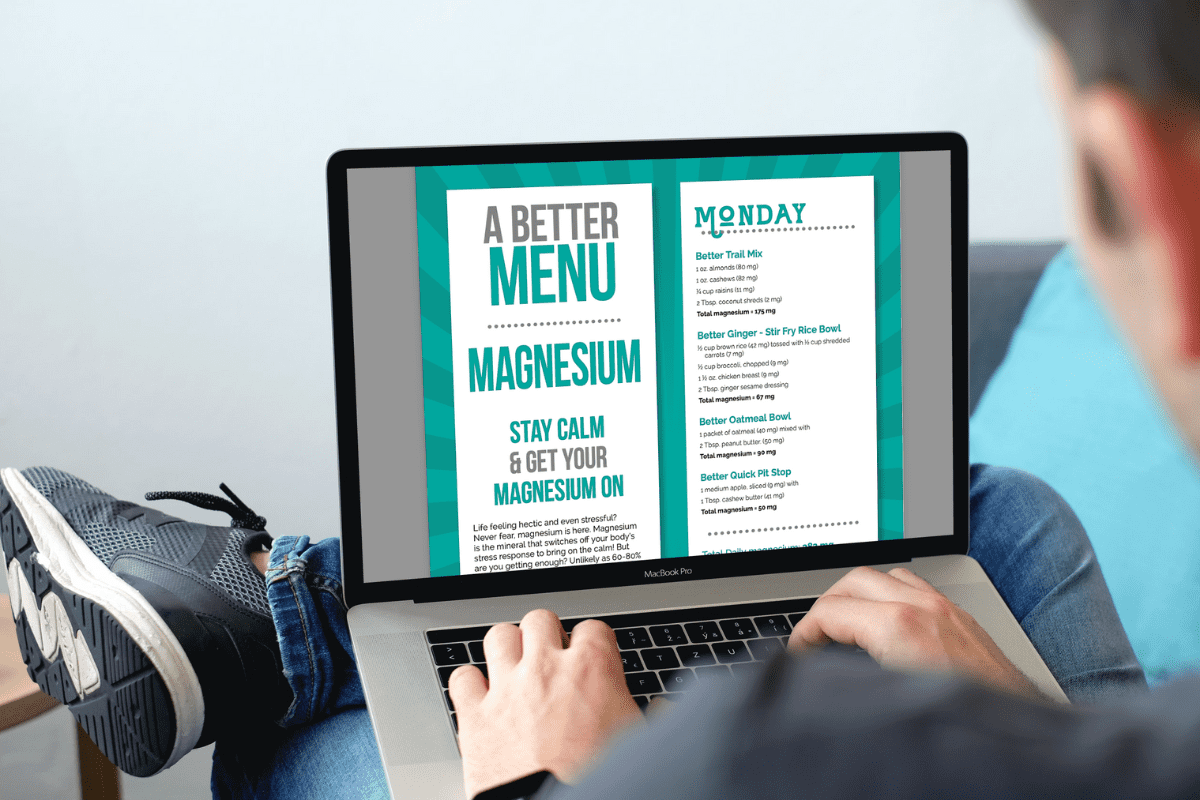
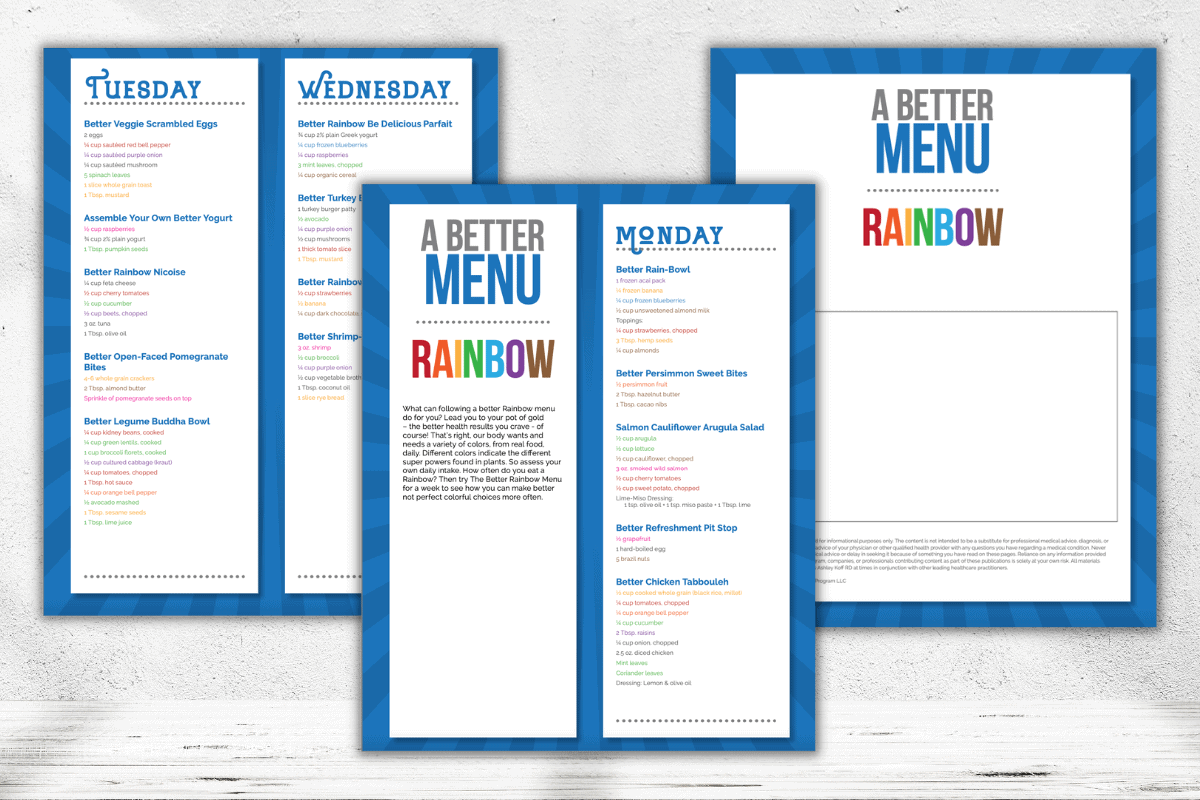
While a continuous glucose monitor reveals data about what is happening, it only gives you partial data on the why. Working with you, a patient can get the whole picture and thus make her truly better choices. For a type 2 diabetic, CGM data reveals that less oatmeal each morning would be better for her blood sugar. However, just reducing oatmeal intake isn’t better overall. That reductions translates to less fiber, B vitamins and magnesium. With better nutrition assessments you can show her this shift. “Your BNP Toolkit™ complements the CGM results to show her what to add not just subtract to truly optimize her total nutrition,” says Koff.
Another win? Helping move clients from a vicious diet cycle to a healthier for them lifestyle.
Diet mindsets can have them stuck thinking of good versus bad foods. You can use a CGM strategically to show them what’s better. For two weeks eating her go-to diet, she can review blood glucose responses as simply information without a “good” or “bad” designation. With detailed notes on what foods your client is eating, when she’s exercising, how well (or not) she’s sleeping and how stressed she feels—all components that impact blood glucose response!—you can help her see patterns that’ll give her incredible insight into her better choices. For example, what happens to a client’s blood sugar when she has a fruit smoothie for breakfast versus one loaded with veggies, avocado, nut butter, and unsweetened almond milk as the base? What happens when someone eats a whole sandwich—versus eating half the sandwich and then the other half three hours later? Or when she adds a pre or post-eating walk into the mix.
“I think it’s great that more people have access to the kind of info a CGM provides. But it’s important to show them that without you – the nutrition professional armed with additional better total nutrition assessment tools – they won’t get a truly personalized plan,” Koff says. “Without you, they are more likely to follow the advice on Facebook groups or from the CGM company they’re using and simply ditch carbs. You can help them do better and make changes that lead to better lasting health.”
Step No. 4: Keep Personalizing by Adding Routine Reassessments
When you’re working with clients who are using a CGM to manage Type 2 diabetes, reassessment and continual changes to their nutrition and medication plans are key. Excellent compliance – often the result of using a CGM to actually see what their choices do – often translates into the opportunity for a reduction in medication. Awesome sauce!
For clients who are using a CGM as more of an experiment, reassessment may not be as crucial medically speaking—but it is an incredibly important piece in helping people create a healthy relationship with food and to tee them up for nutrition success even when they’re not using a CGM.
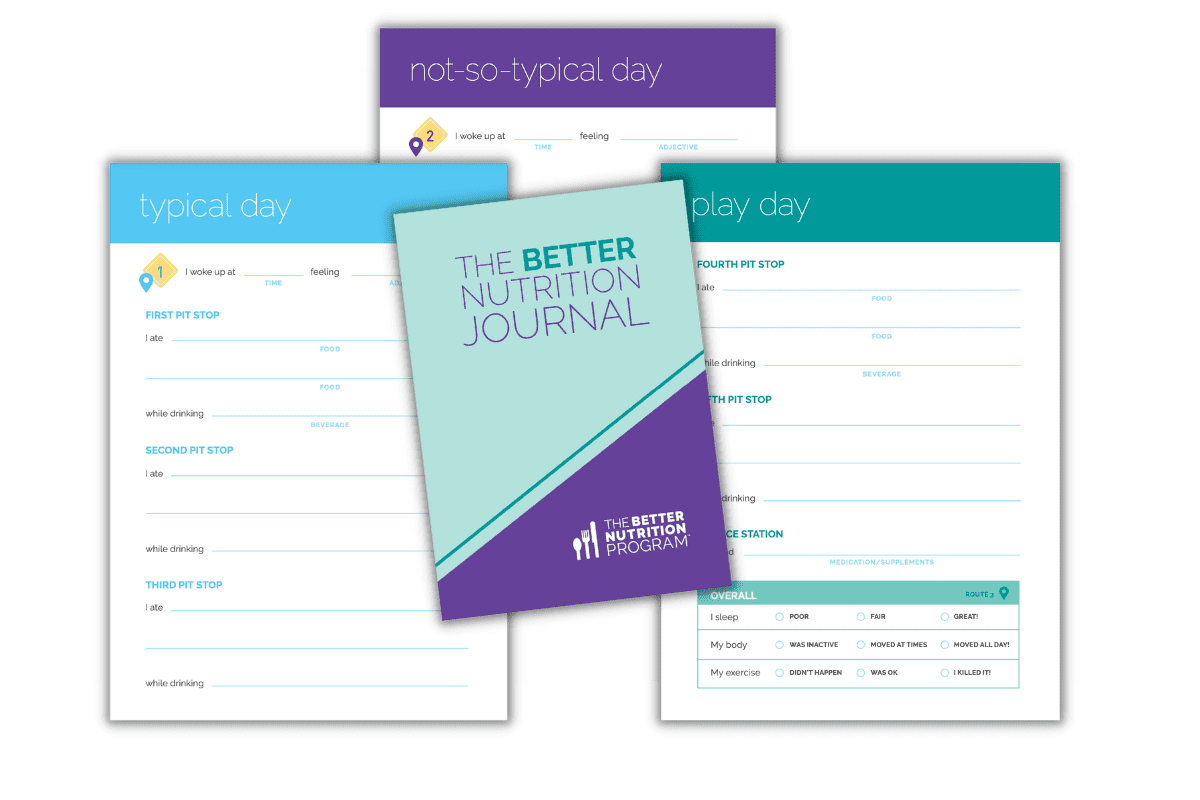
“The ultimate goal for your clients is to discover how all their choices work together, better, for their body. This takes time to implement recommendations and track their impact. Using a CGM, the Better Nutrition Journal, key evaluations, and labs help you personalize most effectively,” says Koff. “The business bonus is that this approach more easily sells packages and helps to ensure client retention. You can divide up your work together into phases: assessment, implementation, monitoring, and optimizing. Once you’ve identified a plan that works for them, move them to maintenance. During this phase you will revisit assessments like the digestive evaluation and repeat the CGM as a seasonal or annual offering.”
Companies with Winning Continuous Glucose Monitor Products Right Now
Currently, CGMs are medical devices, so your clients will need a prescription to purchase one. Currently, four companies have personal CGM devices on the market in this country:
- Abbott (FreeStyle Libre and Freestyle Libre 2)
- Dexcom (the G6)
- Medtronic (Guardian Connect and Guardian Sensor 3)
- Eversense
For clients who want to use a CGM to gain insights into their diet and optimize blood sugar levels, many companies are working the prescription directly into the purchasing process—and sending one of the above CGMs to customers as part of their program. This is a fast-growing field with changes happening frequently. Right now, here are a handful of the companies offering CGMs to non-diabetics:
Companies like Fitbit, Apple, and Google are reportedly investing in CGM technology as well. There’s no doubt we’ll continue to see glucose monitoring become more widely available—and possibly even less invasive. For example, Apple has a patent application for a proprietary technique to non-invasively measure glucose via the Apple Watch. Thus, it’s even more important for nutrition pros to understand how to use information such as blood glucose readings when creating a personalized nutrition plan, says Koff. “And when your clients win at lasting health powered by better nutrition, you win, too.”
Want to up-level your knowledge about blood sugar and continuous glucose monitors—and have all the tools you need to help clients do the same?
All BNP offerings include The BNP Toolkit™ with lifetime access to all the resources you need to offer personalized nutrition. Get the assessments to optimize their nutrient intake along with the done-for-you marketing materials to attract and retain clients.