It’s the most awful time of the month for so many women, with bloating, fatigue, irritability, and cravings making it especially tough to stick to their better nutrition program. The good news: You can help your clients have an easier time by personalizing PMS recommendations. Here’s how.
In this article, you’ll …
- Learn how to personalize nutrition advice for women experiencing PMS symptoms
- Understand why PMS shouldn’t sideline your clients—and find out how to help them realize that, too
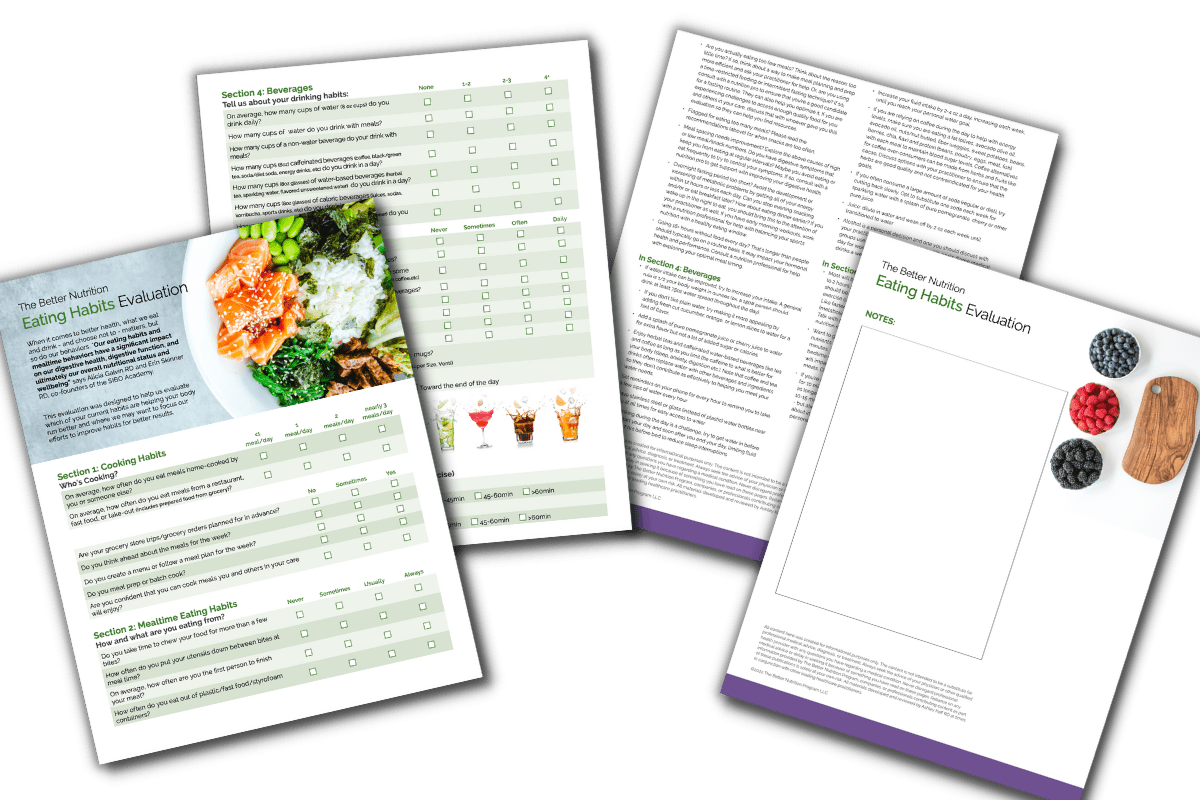
- Get practical tips on incorporating The Better Nutrition Program evaluations into your sessions with clients to help them get better results
- Read about the tactics that can help your clients handle the hormonal flux of the week leading up to their menstrual cycle
Ask women to tell you about the symptoms they experience the week leading up to their period—a.k.a. Premenstrual Syndrome, or PMS—and there’s a good chance the range of answers you get will lean net out at something that resembles “ugh.”
But here’s something that shocks both my patients and the nutritional professionals I mentor: while it’s normal for women to have shifting hormones throughout their cycle, it’s not normal to have the kind of wild, misery-making symptoms so many women deal with.
That’s right. Most women simply accept that the week or so before their periods will be hell, but it doesn’t have to be this way!
And as a nutrition professional, there’s a lot you can do to set your female clients up for success by personalizing your advice based on their PMS experience. In fact, it’s crucial that this happens (and that any given client’s PMS symptoms continue to be assessed!) because of the nature of hormones themselves. After all, one woman’s cycle—and the symptoms that come along (or don’t!) with it—will be different from another woman’s. Not only that, but that woman will likely experience different symptoms in any given month or year.
Given this ever-shifting hormonal landscape, you have a great opportunity to not only assess where your clients are at when it comes to their monthly cycle and hormonally-charged symptoms, but also help those clients understand why they’re experiencing those symptoms.
This is key! So many women feel like a victim of “that time of the month,” changing everything from how they live and who they see to how active they are and what they eat based on the fact that they’re dealing with PMS. And I’m here to tell you that by spending some time understanding your female clients’ menstrual cycle (and helping them understand it better, too!) and then customizing your advice based on what’s happening on that very personal level, you can help your clients move from a place of PMS challenged to having a normal menstrual cycle that doesn’t send their good sleep, exercise, and diet habits out of whack.
First, what exactly is PMS?
Before you start talking to your clients about their experience with PMS, it’s helpful to remember the medical definition. PMS is a catch-all name for the more than 150 physical and psychological symptoms that researchers have pinpointed can happen to women during the five to 10 days before their period begins.
Essentially, a woman’s hormones are shifting drastically during this time—and as a result of those shifts, she may end up with one or many symptoms. Because PMS has such a wide range of symptoms, it’s important that your clients understand “normal” doesn’t exist. That said, severe symptoms could be a sign of a more serious condition, such as PMDD or endometriosis, which means it’s important to urge your client to talk to her doctor if she’s experiencing:
- less than one or more than three bowel movements daily
- low energy, severe cramps, headaches, back aches, intense mood swings, and/or digestive issues that sideline her
- symptoms that interfere with normal activities, if she can’t concentrate, or if she stays home instead of participating in day-to-day activities
When you better understand PMS and all that it can entail, you can educate your clients and help them see your role in helping them navigate this time of the month. Then, you can ultimately help them ease their symptoms with your personalized advice.
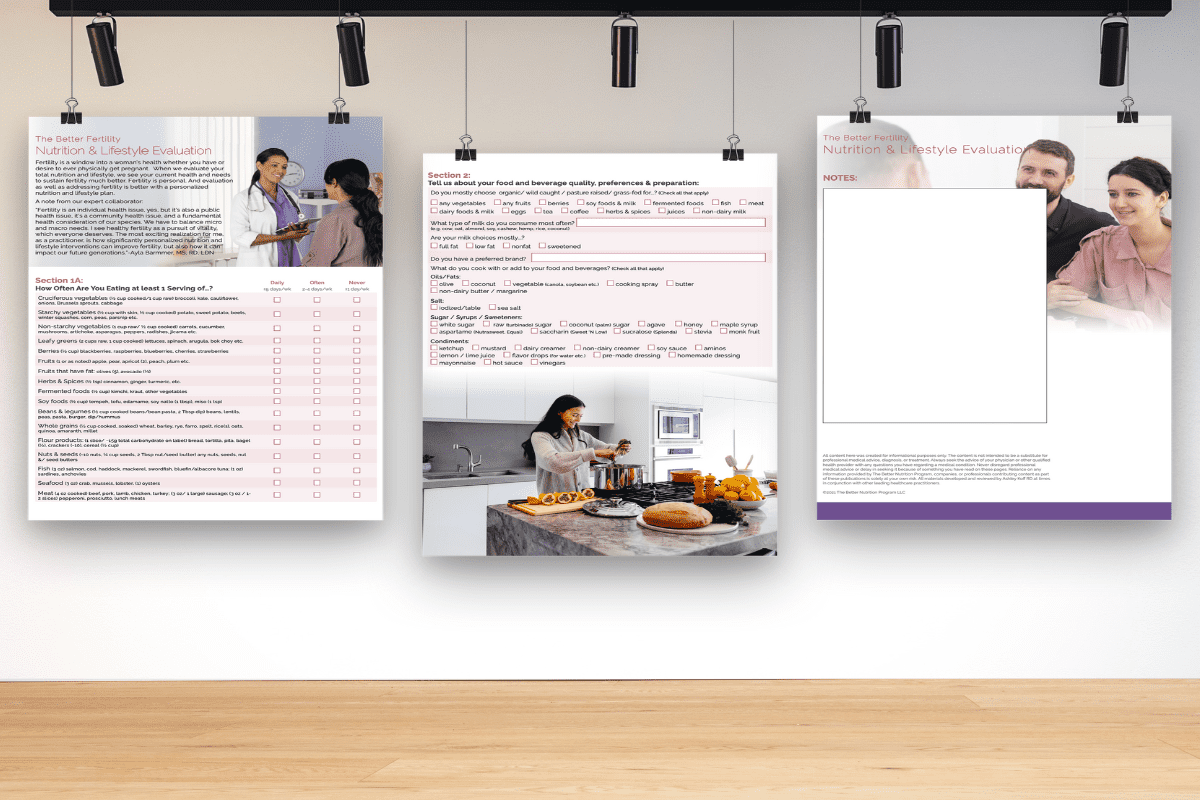
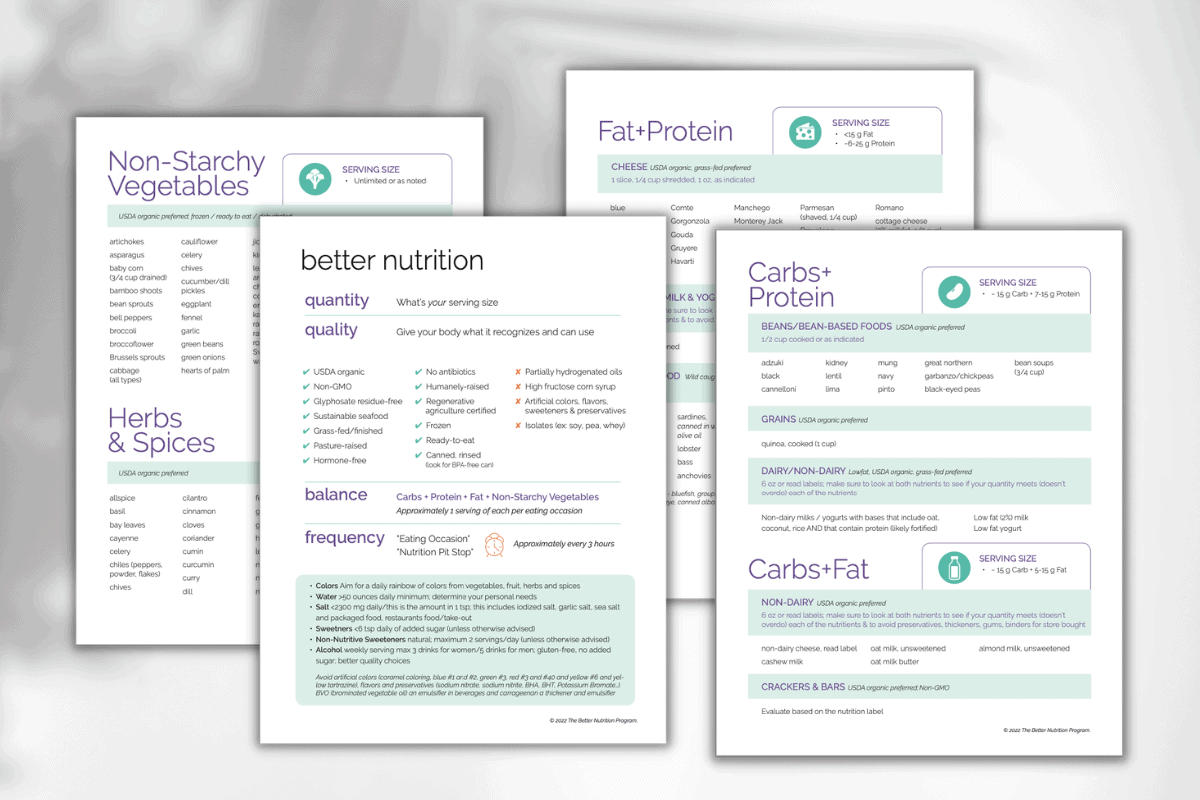
Looking for an easy way to attract prospects or talk to existing patients about PMS? The BNP Toolkit™ includes an expert guide to PMS that helps them understand your value. Share it with them to explain how personalizing PMS recommendations will help them get better results. Thrilled to collaborate with women’s health experts Carolyn Brown RD and Sarah Swanberg DACM of Indigo Wellness on this guide.
3 Keys to Personalizing PMS Recommendations
To help your clients better understand their cycle, the hormonal shifts causing their symptoms and what they can do to sail through this time of the month, here’s my best advice:
1. Ask your clients to track their cycle.
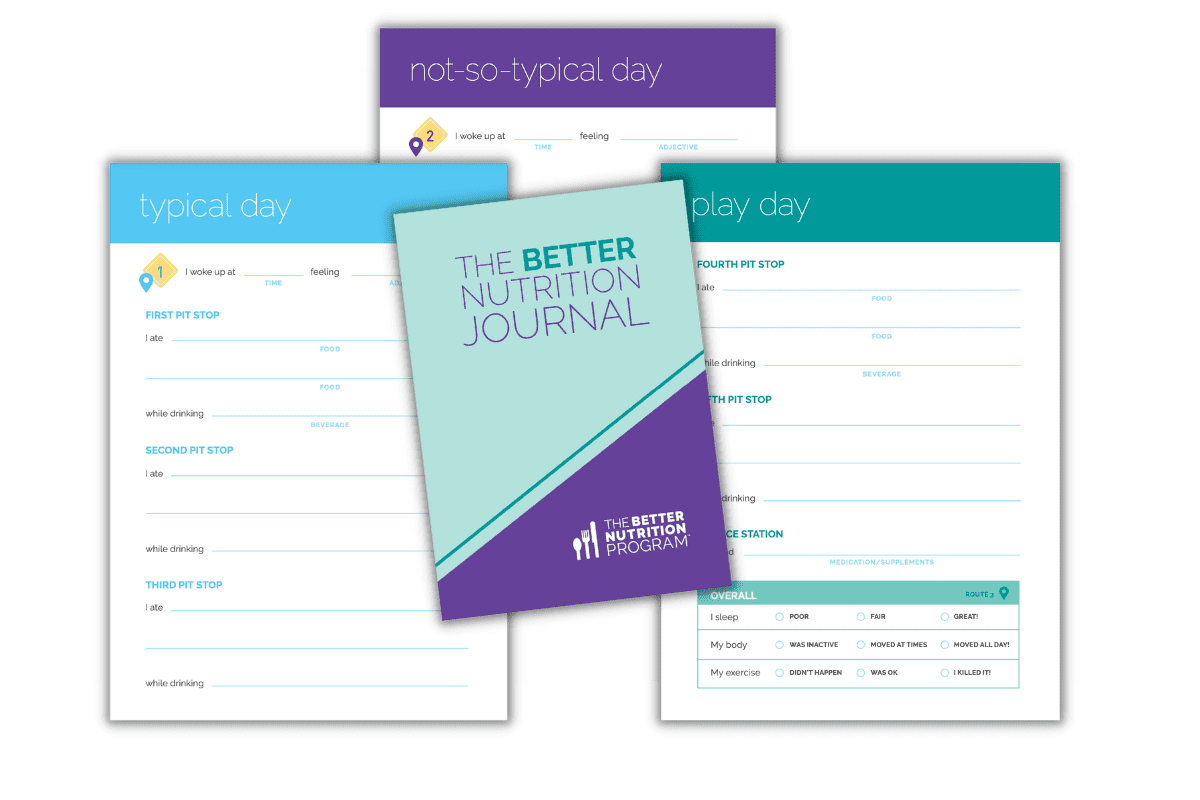
The bottom line is that your patients need to know when they’re dealing with PMS—and what their symptoms look like—to put any of your recommendations into action. I always recommend using a period tracker (there are so many great, free apps these days!) in combination with The Better Nutrition Journal so clients can see what foods, beverages, sleep patterns, and even mood changes happen during the week or so leading up to their cycle.
What’s especially great about The Better Nutrition Journal is that it gives both you and your patients a chance to define what PMS means for sleep, mood, and energy. It’ll help your client understand (and help you clearly see) when changes happen in these areas, and at what consistency. This intel can help you understand what times of the month are prime times to introduce healthy changes, for example—and what times it may be tougher to stick to better choices. When both you and your client are armed with this info, you can help maximize those times when healthy changes will be easier to stick to and offer advice for navigating the trickier moments.
2. Do a Digestive Evaluation…Twice
When hormones shift, they throw digestion off course. And while this is normal, when personalizing PMS recommendations we need to know what these shifts mean personally—for each woman—to help her achieve better digestion, mood, and energy. To get that kind of intel that’ll help you create personalized recommendations, The BNP Digestive Evaluation is key.
My recommendation is that you do this evaluation twice—the first one 10 to 12 days before your client’s cycle starts, and another one to two days after her period has stopped. This can help you identify triggers for poor digestion (and as a result, PMS symptoms!) and give you great intel about how to address them. For example, when you understand when digestion slows down and elimination stops or becomes challenging versus when you are likely to have loose stools or no digestive challenges, you can provide the detailed recommendations that’ll give your clients’ bodies what they need to run better while reducing what can irritate, overwhelm and disrupt those efforts. Understanding this total nutrition for each one of your clients will help you discover deliciously doable—or supplemental, when necessary—choices to them better meet their body’s needs.
3. Understand your patients’ biggest challenges.
When it comes to truly optimizing her nutrition to set her up for lasting success, you have to get to the bottom of what she struggles with the most. This is true when it comes to most aspects of their lifestyle habits, and it’s certainly the case when you’re talking about the hormonal shifts that can lead to PMS symptoms. With all of my female patients, I ask them about what they find toughest during this time of the month—everything from sweet cravings to energy tanking to difficulty sleeping—and after we make a list of those top pain points, I ask them to rank each on a scale of one to 10, with one being very manageable and 10 being torturous. We talk about what each of these struggles is like not just during the week leading up to their period but also the other times, to get a real picture of just how much hormonal changes may be at play. And for the areas that are significantly different during that PMS week, we focus on those things during that time period.
These conversations get really personal, and they can be challenging! After all, you’re talking to clients about things they may not feel they have control over, and what tends to impact their lives in serious, negative ways. Yet these tricky conversations are so important to have, especially because whatever is “off” most times of the month will almost certainly be worse during PMS. For example, if digestion isn’t good as a baseline, that will only be amplified during PMS. On the flip side, if someone feels pretty good throughout the month except that week of PMS, then we can focus on solutions that’ll smooth things during just that week.
5 Recommendations to Help Your Clients Who are Struggling With PMS Symptoms
While personalizing your advice is key, there are a number of tactics that tend to help women across the board. Here are some pro tips:
1. Eat good quality carbohydrates.
Carbohydrates are always our body’s (and our brain’s) preferred source of energy. Carbs are also a key source of essential nutrients that a woman’s body uses in the week before her period, which means personalizing your clients’ plan for carbohydrates is essential. For clients who are on very low-carb diets and experiencing bad PMS symptoms, it’s essential to have a conversation about the right quality and quantity of carbohydrates. Strategizing around this can be a game-changer!
2. Get enough fiber and water.
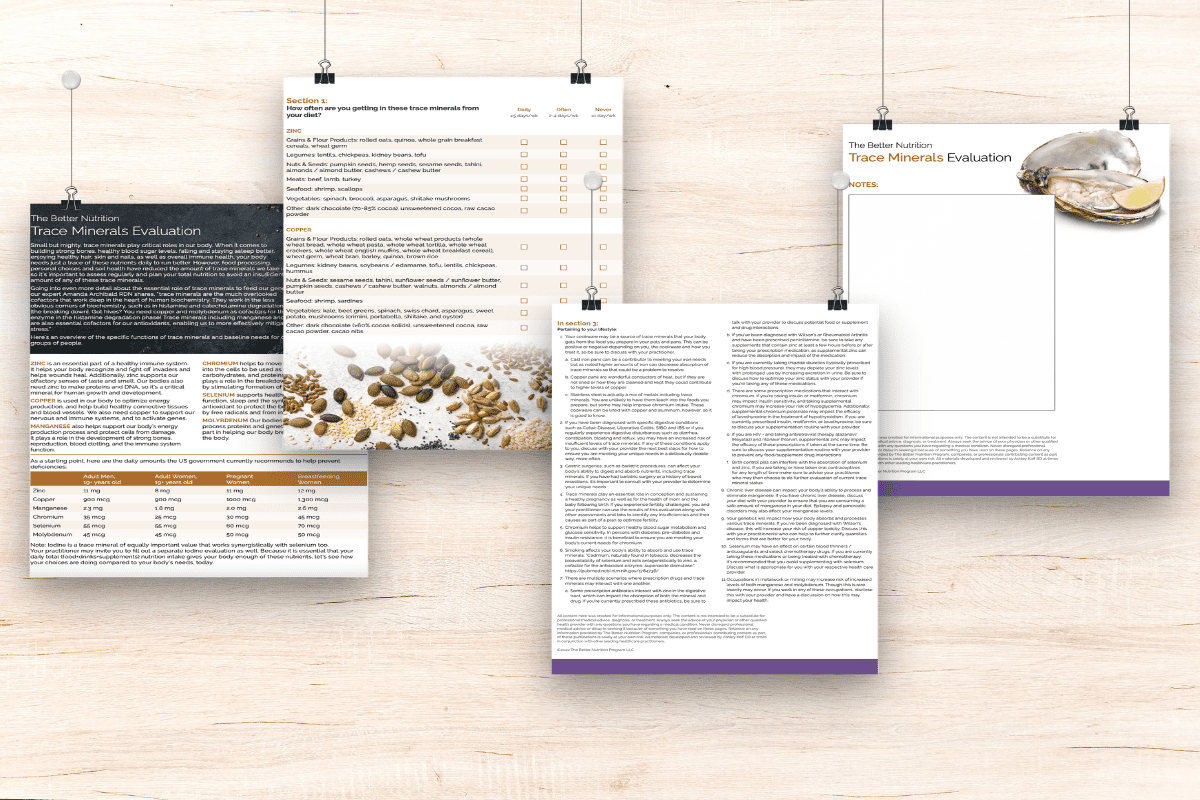
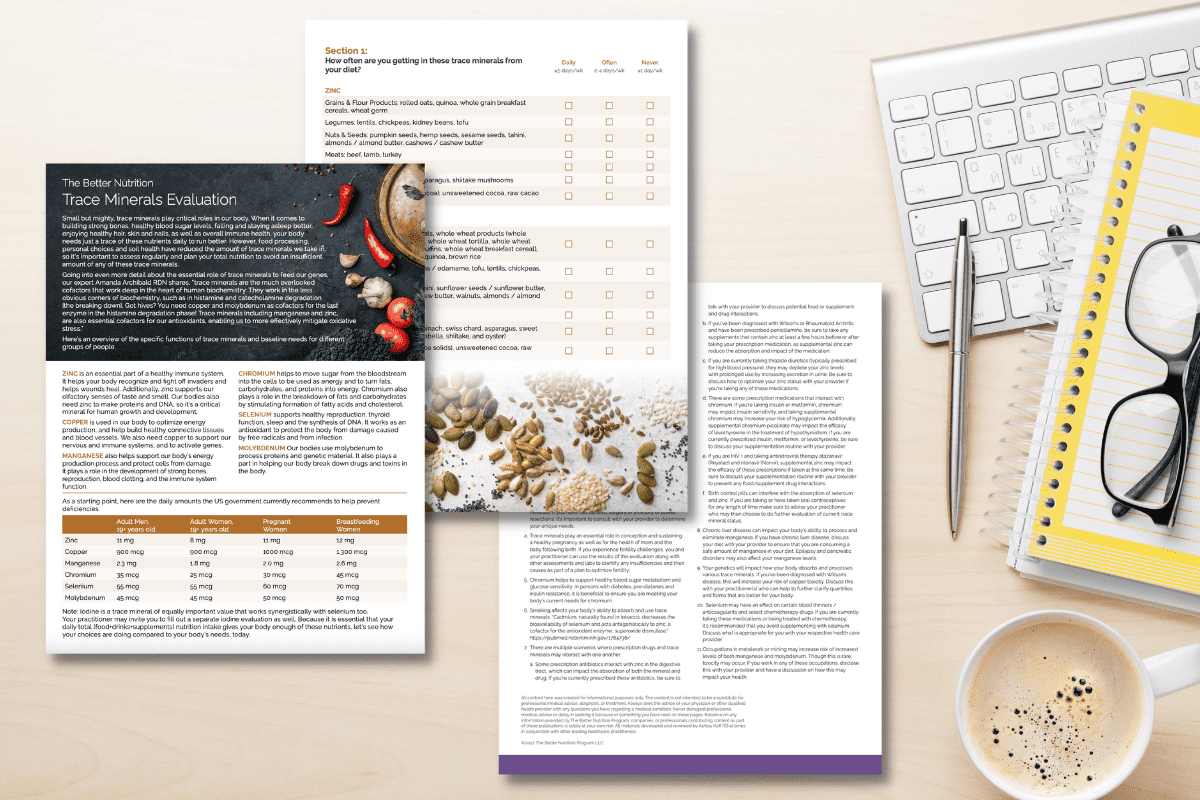
The BNP Toolkit™ includes fiber and water evaluations key for women dealing with PMS symptoms. They’ll help you look at the different types of fiber your clients are including in their diet and how much someone’s having at any one time—crucial info considering fiber’s role in helping to remove used hormones and waste, and to help us feel full (which can be especially helpful in conquering PMS cravings!). That said, when hormonal shifts throw digestion off course, it can mean things really slow down—which in turn can mean that fiber may not move through the body as intended. That’s where making sure your client is drinking enough water can help, as well as shifting fiber recommendations.
3. Reduce caffeine, alcohol, and added sugar (or non-nutritive sweeteners) intake.
Everybody has a different relationship with caffeine, alcohol, and sugar. For many patients, a little extra caffeine, sweets or some alcohol during this time is fine. In fact, caffeine may keep your digestion moving and motivate you to do that workout, while a little alcohol or a few bites of dessert may be part of a dinner out or time with a friend. But the opposite can occur too. Alcohol can exacerbate depression and fatigue, interfering with already challenged sleep and moods. Caffeine can prompt you to push your body further than it wants and interfere with sleep. And too much sugar can mess with your already impaired digestion, not to mention send you on a blood sugar roller coaster that’ll wreck your mood. When it comes to these treats, it’s especially important that you and your practitioner personalize better choices. The way to do that is to assess their impact and try adjustments when your nutrition and lifestyle choices support your body to make it easier.
4. Make sure your total nutrition is delivering enough B vitamins and choline.
In an ideal world, your clients’ food sources will deliver the right amount of these crucial nutrients. If that’s not the case, you may need to supplement. Here’s why B vitamins and choline are so crucial when it comes to PMS symptoms: mood, energy, digestion, muscle cramps, fertility, metabolism and methylation all rely on sufficient intake of several B vitamins plus choline. Use The Better B Vitamin Evaluation (part of The BNP Toolkit™) to see if your client is getting enough, which in combination with lab results and genomic testing can help further determine which sources and amounts your client’s body needs to run better.
5. Eat the rainbow.
This advice may sound simple, but eating the rainbow of colors from fruits, vegetables, herbs and spices helps the human body run optimally. From greens like broccoli that help with removing used hormones, to anti-inflammatory support of a whole range of colors, and potassium-packed white foods like cauliflower, the rainbow helps her body do what it needs to throughout the month. Spices, herbs and supplements may help her get in a rainbow more easily. Your BNP Toolkit™ also includes The Better Rainbow Evaluation and Rainbow Menu, as well as other tools to make this easier to show her her better choices. Use these to personalize her PMS and all month long recommendations to get the many benefits of nature’s colors.
Help her and here’s how your business wins too!
Of course, helping patients is our primary goal, our raison d’être (reason for being), right?! But it is also great for your business too. Developing her protocol can take several months. Each month you can assess how new tactics and better nutrition is helping her body. This helps you piece together a winning plan. And when explained this way, helps her see why investing with you for 3,6,12 months is better.
Want to preview The BNP Toolkit™ that makes personalizing PMS recommendations and marketing it easier and more effective? Join us for a live demo.