For decades, heart health advice has centered on a core idea: Lose weight to reduce risk.
But weight loss and heart health are not reciprocal actions: if you lose weight, you become heart healthy.
Weight loss focuses on reducing total body weight. Weight health focuses on optimizing how the body functions.
It is entirely possible to lose weight while losing muscle, worsening dehydration, blood sugar, digestion and stress hormones, and impairing metabolic health overall. All of these outcomes detract from cardiovascular function.
Why Scale Weight Is a Poor Measure of Heart Health
Total body weight does not indicate what that weight is composed of. That’s because a basic scale can’t distinguish between:
- Muscle and fat
- Subcutaneous fat and visceral fat
- Water inside cells versus fluid outside cells
Two people with the same weight and BMI can have very different heart health profiles. One may have strong muscle mass, stable blood sugar, and low inflammation, while the other may have high visceral fat, insulin resistance, and vascular strain.
Individual differences are why weight alone fails as a predictor of cardiovascular risk.
Visceral Fat Matters More Than Total Weight
Visceral fat, stored around your internal organs, is one of the strongest drivers of heart disease risk. Visceral fat produces inflammatory compounds, disrupts insulin signaling, and increases strain on blood vessels and the heart.
Reducing visceral fat improves cardiovascular outcomes even when total weight loss is slight. Losing weight without reducing visceral fat doesn’t offer the same protection.
Muscle, Hydration, and Metabolism Support the Heart
But optimal heart health depends on more than fat reduction. Muscle mass improves glucose regulation and reduces cardiovascular workload. Hydration and electrolyte balance support heart rhythm and blood pressure control. Metabolic flexibility allows the heart to adapt to changing energy demands.
Weight-loss strategies that reduce muscle or compromise hydration may lower the scale reading but increase cardiovascular stress.
Digestion and Electrolytes Are Overlooked Heart Health Factors
Digestion plays a critical role in heart health. The heart relies on nutrients absorbed through the digestive tract, including magnesium, potassium, amino acids, and fatty acids. If digestion or absorption is impaired, the heart may be under-resourced even with a “heart-healthy” diet.
Electrolytes, particularly potassium and magnesium, are essential for:
- Heart rhythm
- Vascular tone
- Blood pressure regulation
Weight-loss approaches that restrict intake or impair absorption can unintentionally disrupt these systems.
Weight-Health Hormones Link Weight Health and Heart Function
Weight-health hormones such as GLP-1, GIP, PYY, and CCK coordinate appetite, digestion, metabolism, inflammation, and cardiovascular signaling.
These hormones have receptor sites in:
- Heart muscle
- Endothelial tissue (lining of the arteries)
When weight-health hormone function is optimal, cardiovascular efficiency improves. When it is impaired, heart health suffers regardless of body weight.
This explains why improving weight health often leads to better heart outcomes even without dramatic weight loss.
When Weight Loss Without Functional Improvement Backfires
Weight loss without improvements in function can:
- Increase stress hormones
- Reduce muscle mass
- Worsen hydration and electrolyte balance
- Impair hormone signaling
In these cases, the scale may move while heart health stagnates or declines. This pattern also helps explain why weight regain is common and cardiovascular risk often persists.
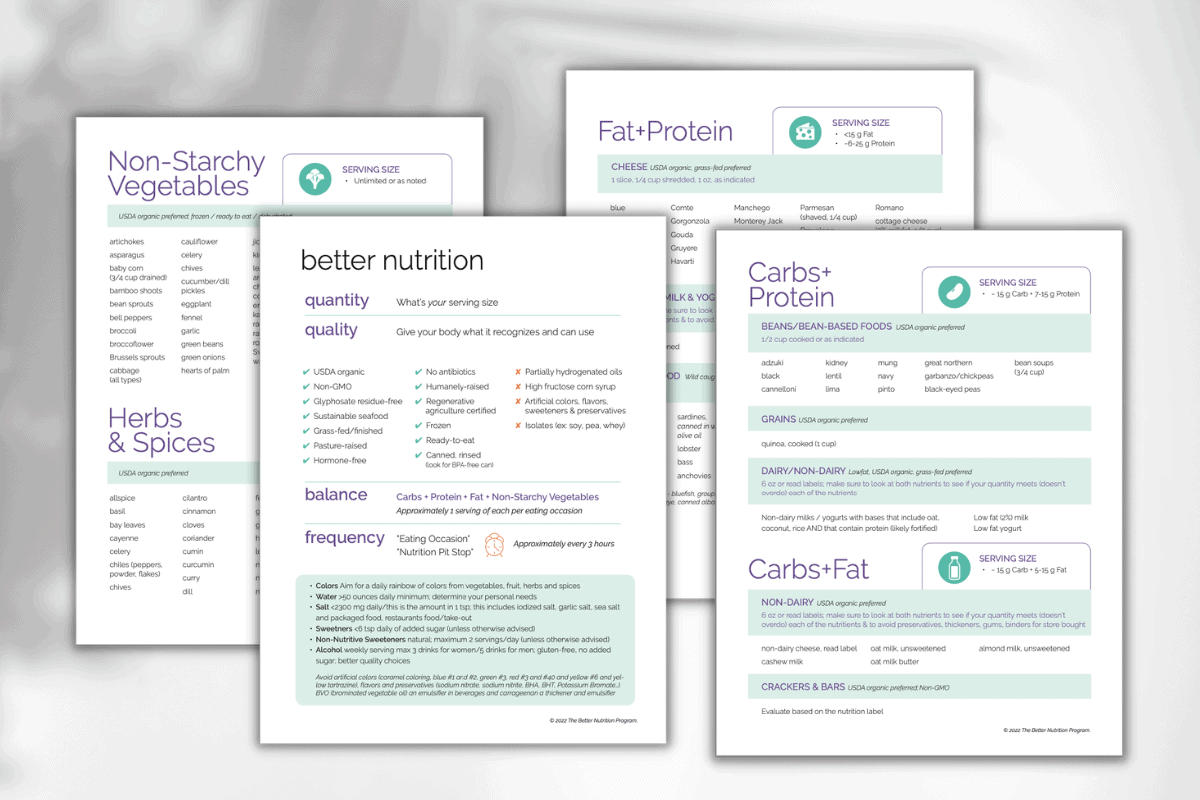
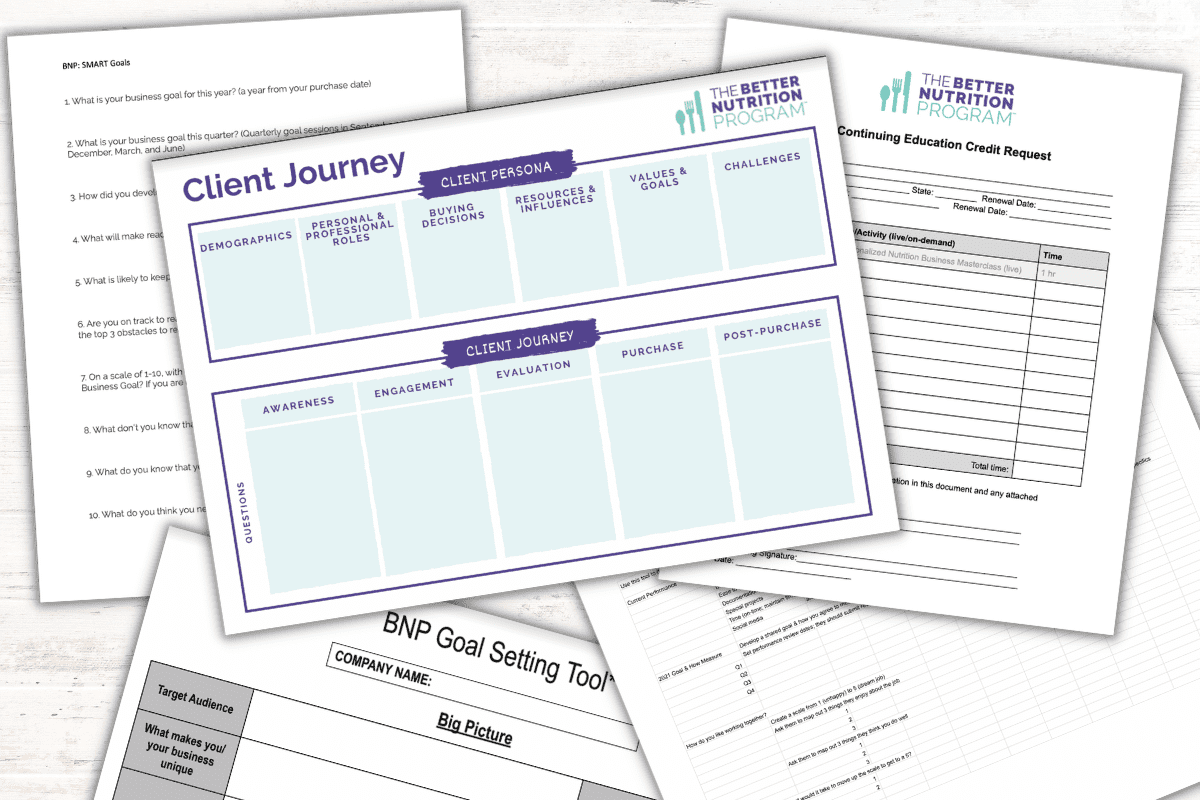
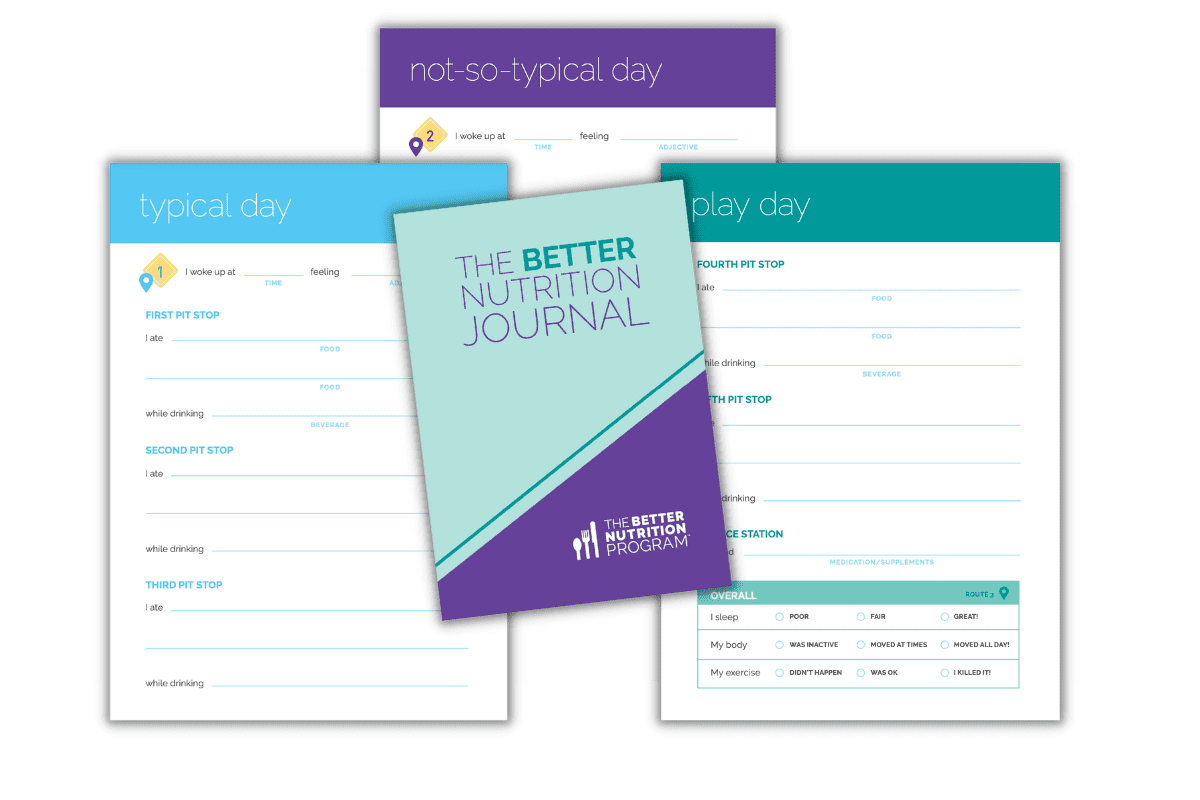
The BNP Approach: Improve Weight Health to Improve Heart Health
At The Better Nutrition Program, we address heart health by improving your weight-health ecosystem.
We assess:
- Body composition rather than scale weight
- Visceral fat patterns
- Digestive function and nutrient absorption
- Hydration and electrolyte status
- Metabolic and inflammatory markers
- Weight-health hormone signaling
When these systems improve, weight may change naturally. More importantly, heart health improves in measurable, meaningful ways.
The Takeaway
Weight loss is not a reliable proxy for heart health. Weight health is.
A heart-healthy body:
- Preserves muscle
- Manages inflammation
- Maintains hydration and electrolyte balance
- Supports hormone signaling
- Uses nutrients effectively
Improving how the body functions is the key to protecting the heart over the long term.
Heart Health FAQs
What is the difference between weight loss and weight health?
Weight loss focuses on reducing total body weight, while weight health focuses on weight composition — the amount, type, and location of muscle, fat, bone, water – as a signal of overall health, one of many that informs operational status.
Can you improve heart health without losing weight?
Yes. Improving muscle mass, reducing visceral fat, optimizing digestion, supporting hydration, and improving metabolic and hormone function can all improve heart health without significant weight loss.
Why is visceral fat dangerous for heart health?
Visceral fat produces inflammatory compounds and disrupts insulin signaling, increasing strain on blood vessels and the heart, even when total weight appears normal.
How does digestion affect heart health?
The heart relies on nutrients absorbed through digestion. Poor digestion can limit magnesium, potassium, and other nutrients essential for heart rhythm and vascular function.
Do GLP-1 hormones affect the heart?
Yes. Weight-health hormones like GLP-1 have receptor sites in heart muscle and arterial tissue and influence cardiovascular function beyond appetite regulation.