To supplement or not to supplement – that is NOT the question to answer when it comes to optimizing iron levels for each person. Whether vegetarian, pregnant, fitness fanatics or living with certain medical conditions, your clients need optimal iron levels for their bodies to run better. They may come to you suspecting low iron levels or with a diagnosis of iron-deficient anemia. What else should be considered when working with clients with iron-related issues? In this article, you’ll learn:
- How to personalize iron recommendations that yield better client outcomes
- When to recommend an iron supplement, and when to offer alternative solutions
- 8 frequently-asked iron-related client questions to help you
Iron is a vital and complex nutrient, and is often oversimplified in conventional settings. It’s true that iron deficiency is common, especially among certain groups, including women.
“It’s time to break up with the notion of “low iron, take a supplement.” There is so much more we need to assess to understand the root cause of iron insufficiency or frank deficiency, and to determine the better protocol for each patient.”
Ashley Koff RD
Why shouldn’t you recommend a supplement for a low iron lab result?
Automatically recommending an iron supplement may mask other nutrient insufficiencies or excesses. A supplement can also exacerbate issues such as digestion and inflammation, which ironically may be tied to their low iron. And a supplement is only one part of total nutrition. You will want to look at their food, drinks, other supplements, medications and even skincare to optimize iron levels for better overall health outcomes.
How can I personalize iron recommendations?
“I request labs to get a more comprehensive understanding of their health. I send them The BNP Iron evaluation with the lab request to help me get the most complete data.”
Ayla Barmmer MS RDN LDN, founder of FullWell Fertility
To gain a more accurate picture, order labs (see below) and simultaneously, assess total nutrition and lifestyle. You can also start with an iron nutrition assessment as it could give you directional data about additional labs (stool, micronutrients, hormone etc.) to request.
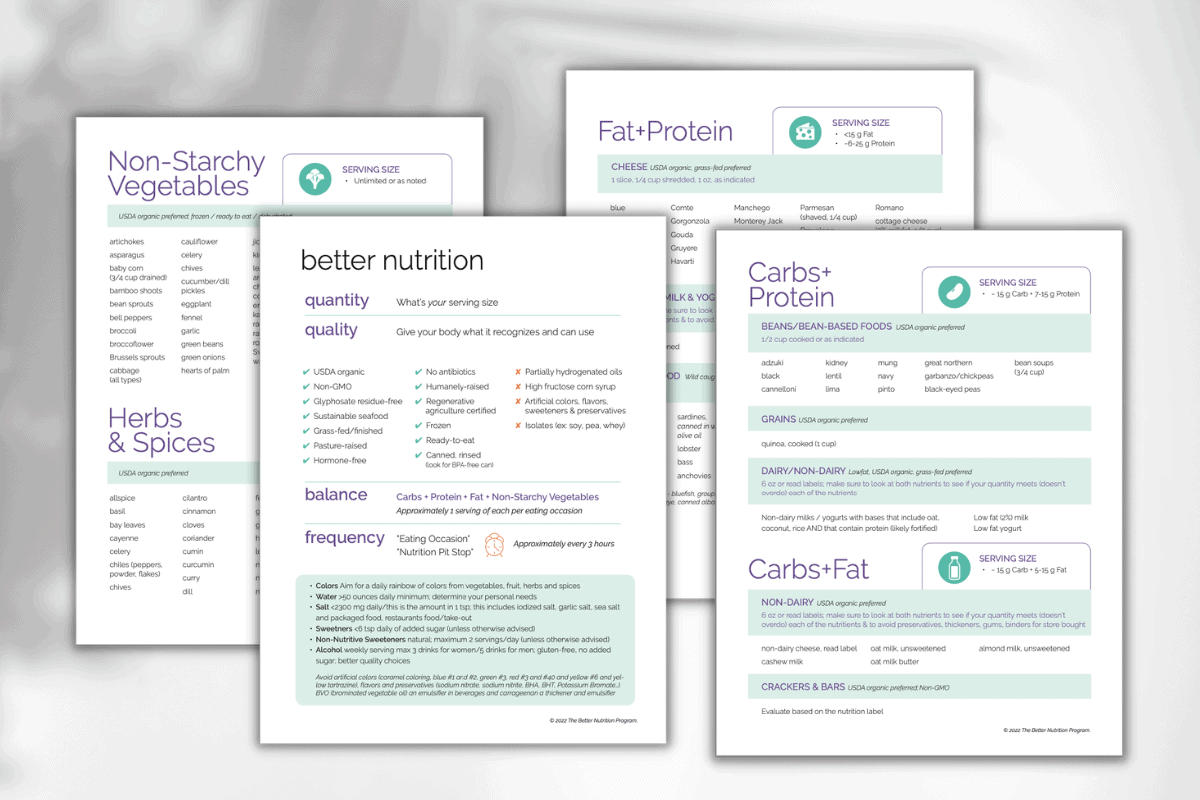
Our Iron evaluation is a valuable tool for your practice (get it with lifetime access as part of The BNP Toolkit™, is helpful at this stage to provide greater insight into the client’s diet, lifestyle, medications-anything that may be influencing their iron status.
What labs should be ordered to properly assess & optimize iron levels?
Our experts recommend the following for data:
- Iron and CBC panels, at minimum.
- Checking ferritin levels can tell you a lot about the client’s stores and can be a great early indicator of iron status.
- You may also want to look at TIBC / UIBC
- Also, ordering a C-Reactive Protein (CRP) panel can also provide more information. CRP is not something typically thought of having a relationship with iron. But, if you are looking at ferritin, it’s also helpful to look at CRP because inflammation and a high CRP can make ferritin look falsely elevated.
Will foods alone optimize iron levels?
It depends on several factors. Is the person willing to eat the food, and enough of it? Will their digestion work effectively to share the iron where needed? Are they getting in nutrients that support better iron absorption?
Share these questions as part of building each person’s recommendations to optimize their blood levels. Instead of an iron supplement, you may be introducing them to more vitamin C rich foods and recipes that combine them with iron. Likewise, you could be recommending a digestive enzyme to take with meals to optimize overall nutrient absorption. When you explain what you are doing and why, show them options, and build a plan with re-assessment you are more likely to get excellent compliance and results.
BONUS: The BNP Iron Evaluation and menu don’t just help you assess iron needs and see potential issues, they help you show each patient options – so the patient can make their deliciously doable choices – and for you both to re-assess at regular intervals. This helps you both figure out what works – and doesn’t – for each person!
Dietary intake looks good for iron, but the labs are problematic. Now what?
Before suggesting supplements, it’s best to try and adjust diet first. If dietary intake is good for iron and the labs are still problematic, there are many factors that could be affecting iron status, including digestion, inflammation, bleeding, fitness. Start thinking about the other nutrients that are heavily involved in iron and metabolism, including:
– Vitamin A, which data shows that the majority of women are not getting enough of, helps release iron from ferritin stores.
– Vitamin C enhances absorption of iron. Do they get in enough vitamin C (especially from foods)?
– Copper is essential for absorbing iron in the gut. Low copper can be due to a lot of things. For example, right now many people are taking high doses of zinc for immune support, but if taken over the long term, that can lower copper levels.
You will also want to explore foods, drinks and supplements whose ingredients could be blocking iron absorption from food and supplements (calcium, zinc, caffeine etc.).
When is it ok to recommend an iron supplement?
Any time a patient can not meet their needs with food and beverages, a supplement can help! We are not anti-supplement, We just want to help you make sure the supplement you choose for each patient will be effective for optimizing their iron levels and delivering better health.
There are many different forms of iron found in supplements. Ferrous salts like ferrous fumarate, ferrous sulfate, and ferrous gluconate are typically recommended for better absorption. Some products also include ingredients to optimize absorption.
As you continue to personalize iron recommendations, keep in mind there are some frequently asked client questions (we share some below) that you can use to both attract patients who want your help with personalizing iron recommendations as well as to help those you already work with – here are some of them …
Am I getting enough iron from my plant-based vegetarian or vegan diet?
Not eating meat and worried about giving your body enough iron? No problem, you don’t need to eat to get in enough iron. Plus, while we need iron, excess iron in the body is a health risk. So, for a healthy person, the best way to get iron is through your diet, first, then, with a better quality supplement that adds in what your body needs to run better more often.

How do I know if my iron levels are ok?
Share with patients that they likely need more than an annual CBC to truly optimize iron levels for their body. Also note that life stage changes (planning to be or pregnant, menopause), and training for or performing a significant physical event, are times to check levels and total nutrition, and they should share any of these whether planned or not.
What does iron do in the body?
Iron is part of your better energy team. Hemoglobin, an iron-containing protein of your red blood cells, picks up and delivers oxygen throughout the body. Metabolism, the breaking down of nutrients into usable energy, requires iron. Your immune system also benefits from iron.
How can I have too much iron?
The body can accumulate too much iron from excess intake (typically more of a risk from supplements and fortified foods, not foods, unless one is mono-eating iron rich foods in high quantities). The body can also hold on to iron or not use it when something is not functioning properly.
What is the risk of too much iron?
Excess body stores of iron, as well as “free floating” iron, increases risk of major diseases from cancers to heart and diabetes, as well as concerns of worsening cognitive diseases like Alzheimer’s and Parkinson’s and even speeding up cellular aging (makes sense when we understand what iron does).
What’s the best way to get enough iron?
From whole food first, and from plants first. This can be controversial as there are two types of iron – heme (animal) and non-heme (plants). Over the decades, nutritionists have advised against non-heme sources for absorption concerns. But today we know a few things:
The overall health benefits of plant-based diet.
That other animals get their iron from plants.
That vitamin C and other plant nutrients aid absorption of iron. That, perhaps, the absorption issues of non-heme are a built in protection against too much iron.
Now, that doesn’t mean you can’t enjoy quality animal sources of iron but you don’t need to eat meat to get sufficient iron. Second, during growth phases, as mentioned above, or along with being monitored by your practitioner, during intense periods of fitness and muscle exertion, you may need more iron than you can get in from food alone. Your practitioner may recommend a supplement. Third, when lab values are concerning, your practitioner should conduct a total iron nutrition assessment and may request additional labs to determine root cause. They can then personalize a recommendation for you.
What are the best foods to get enough iron?
Your pulses (lentils, chickpeas, beans etc), hemp hearts, cooked spinach (Popeye!!) and other dark leafy greens, as well as olives, pumpkin and sesame seeds. Whole grains like bulgur, barley and quinoa contain nice amounts of iron (1-2mg per serving, typically 1 cup) and cereals made from these will contain iron as well. However, flour-based cereals are often fortified with iron, one serving can deliver an adult daily dose of iron or more and I like these less (we often eat more than one serving and we hopefully get other sources of iron in the same day). When eating animal sources of iron such as pork liver and mollusks like oysters top the list joined by beef (and beef liver), as well as quality fish like wild salmon. You can also get extra iron by preparing your food in a cast iron pan.
I’m eating iron rich foods and taking a supplement but my levels aren’t getting better.
What can I do? First, work with practitioners who are willing to look at additional labs as well as conduct a total nutrition assessment to get to the root cause . There are factors that can interfere with iron absorption like foods and supplements (coffee, calcium in foods as well as supplements and medications), as well as digestive issues and excess inflammation.
My iron supplement is making me constipated
I can’t keep taking it. This is really common. There are some supplements that work to address this with herbs which also include vitamin C which in addition to promoting better iron absorption can also help address constipation. Your practitioner should assess your magnesium nutrition too as it can help improve motility, and may be needed when adding an iron supplement.
Here’s a favorite iron-rich recipe: Quinoa Medley Bowl


I really like it that you mentioned that the best iron supplements also contain vitamin C, magnesium, and herbs to keep the tummy healthy and moving. This is just what my dad needs to supplement his high-fiber, low-salt, and low-carb diet due to his diabetes. He needs an extra boost of vitamins and irons to replenish the blood he loses from losing sleep every night due to overthinking. I’ll make sure to buy him a bottle of this capsule for one month’s supply.
So glad you liked the article! Make sure you/your dad confirms with his doctor that he needs additional iron before taking any supplement.
Awesome article! I can relate to this from my own journey with chronically low iron. My low iron levels were due mostly in part to a SIBO infection. Therefore supplementing as I had been years before was not helping. Once the infection was cleared up, I was better able to absorb and utilize the iron rich foods I was eating and the liquid iron supplementation.
Thanks again for the wonderful information!
thank you Michele! We love hearing this and so proud of you for your personalized health win!
– Ashley Koff RD