When most people think about heart health, they think about cholesterol, blood sugar, blood pressure, and hip-to-waist ratio.
While these markers can offer useful information, they do not tell the whole story. Focusing on them alone is one reason heart disease remains the leading cause of death in the United States, despite decades of medications, guidelines, and “heart-healthy” advice.
That’s because heart health isn’t about a single lab value or organ. It’s about how well your body is functioning as an ecosystem.
Why Heart Disease Is So Common and Misunderstood
Traditional heart health guidance focuses on parts rather than processes. If cholesterol falls within range, the heart is assumed to be healthy. If blood pressure is controlled, concern often stops there. If BMI looks acceptable, deeper questions may not be asked.
But the heart, like every organ and cell in your body, does not operate independently. It’s part of a weight-health ecosystem constantly responding to signals from digestion, hormones, hydration, inflammation, metabolism, and stress. When any part of the ecosystem functions sub-optimally, your heart is often impacted before numbers move outside a reference range.
Likewise, heart disease risk is also chalked up to being “genetic”. While we share genes with family members, our body has its unique design. And genetics is only at most half of the story.
When practitioners or individuals judge heart health based solely on lab values and genetics, follow recommendations, and take their medications, many still experience declining cardiovascular health.
The Limits of Cholesterol, Blood Pressure, and BMI
Here’s the thing: cholesterol and blood pressure are outcomes, not root causes. Whereas total weight and weight for height are not markers of any internal health status.
Lowering any one number does not automatically restore optimal function.
BMI fails to provide any insight about your body composition, visceral fat, muscle mass, hydration status, or inflammation. It can’t tell you whether the heart muscle is resilient, whether blood vessels are flexible, or whether metabolic health is improving.
Weight-Health Hormones and Their Role in Heart Function
One of the greatest things about GLP1 agonist medications is that research in people taking them is revealing how our bodies are designed. Turns out we are designed with receptors (the destination of and activity point for) for weight-health hormones like GLP1 and GIP.
We now know that it includes the lining of our arterial walls (the same place where plaque becomes a concern) and the heart muscle.
Weight-health hormones, including GLP-1, GIP, PYY, and CCK, are typically discussed and prescribed only in the context of appetite or weight loss. However, they play a role in cardiovascular health. Remember, we are an ecosystem.
That some of these hormones have receptor sites on the heart muscle and the lining of blood vessels means they influence heart contraction, vascular tone, blood flow, and inflammatory signaling. When weight-health hormone function is impaired, the heart works harder and less efficiently, even if cholesterol levels appear normal.
Optimizing heart health requires optimizing these hormones — with or without medication.
Why Digestion, Hydration, and Inflammation Matter for Heart Health
The heart also relies on what the digestive system can absorb and deliver.
If digestion is compromised, key nutrients required for heart muscle function, vascular integrity, and energy production may not reach the bloodstream. Hydration and electrolytes, particularly potassium and magnesium, play a direct role in heart rhythm, blood pressure regulation, and muscle contraction.
Inflammation, whether driven by gut dysfunction, blood sugar instability, or chronic stress, alters how blood vessels behave and increases cardiovascular strain. There are two phases of the inflammatory response – action and resolution – both requiring nutrients in the desired form to be present and usable.
Heart health isn’t just about what you eat. It’s about what your body can use.
A Systems-Based Approach to Heart Health
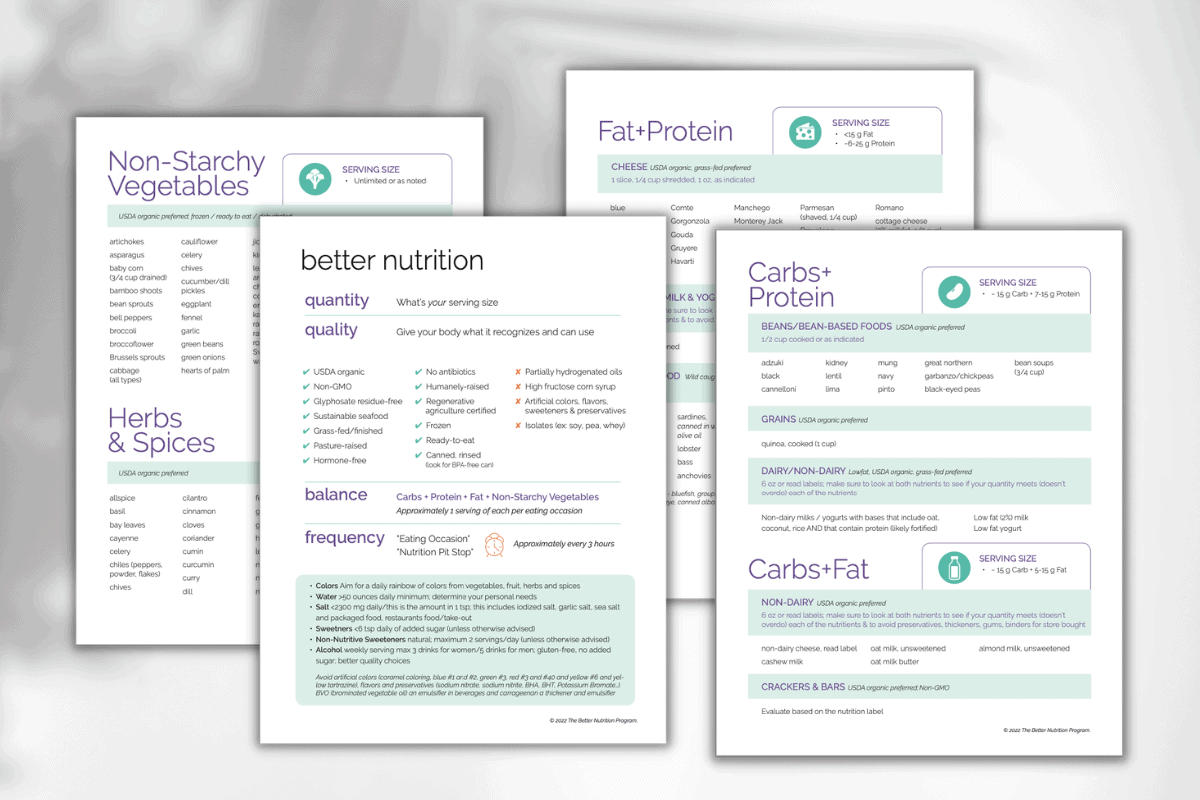
At The Better Nutrition Program, heart health is approached through an understanding of all of the body’s systems, not silos.
Our BNP health plan includes total heart health assessment:
- Digestive function (4 phases)
- Hydration and electrolyte balance
- Inflammation and blood sugar
- Weight-health hormone signaling
This approach doesn’t replace your doctor’s care. It optimizes it. Your doctor may identify suboptimal function. We help you determine how your current choices are contributing and what new choices could restore your body to optimal function – to ensure heart health today and tomorrow.
The Takeaway
Heart health can’t be reduced to whether cholesterol and other lab values are “normal”. Instead, it’s a reflection of how well the body’s systems work together to support cardiovascular function.
Improving heart health means looking beyond isolated numbers and understanding the signals your body is already sending.