Maybe you’ve been told that you’re prediabetic because of an A1C hemoglobin blood test result. So you start paying more attention to how much sugar, even how many simple carbohydrates you’re eating. You’re ditching the Ding Dongs and whacking the white bread. More protein. Healthy fats. Fruits and veggies.
Next year you go back and – dang it! – your A1C is still in the prediabetic range. You might be frustrated and that’s understandable. What you didn’t know is that there are at least 40 factors that affect your blood sugar and only about 10 of them are food-related. Surprising. We know. Because what you hear all the time is that you have to control your sugar and simple carbs. And that’s what you did.
The human body is a complex machine powered by interdependent physiological, biochemical, and anatomical systems. This is metabolic function. Sleep, hormones, hydration, activity, diet, digestive health and more all impact your metabolic function.
Elevated blood sugar is a signal that you’re experiencing metabolic dysfunction. Some other signals include:
- If your digestive system is not functioning properly (reflux, loose stools, etc.)
- Inflammatory skin response – acne, rosacea, other conditions
- Fatigue
- Excessive Thirst
- Hungry all the time
- Cravings
When the body sends us signals, it’s trying to warn us that it doesn’t have what it needs, that your cells don’t have what they need to function properly.
The A1C Lab Result
The A1C provides a reading on a 3-month average of your blood sugar levels. This is better information than a single-point-in-time finger prick test. But still, it doesn’t reveal whether you’re having high peaks and low valleys of blood sugar levels or you’re having a more moderate fluctuation. And if you remember that there are 40 factors that affect blood sugar, we also don’t know what exactly is causing the blood sugar spikes. So don’t feel bad that you didn’t move the needle on your A1C by being “good” with your diet.
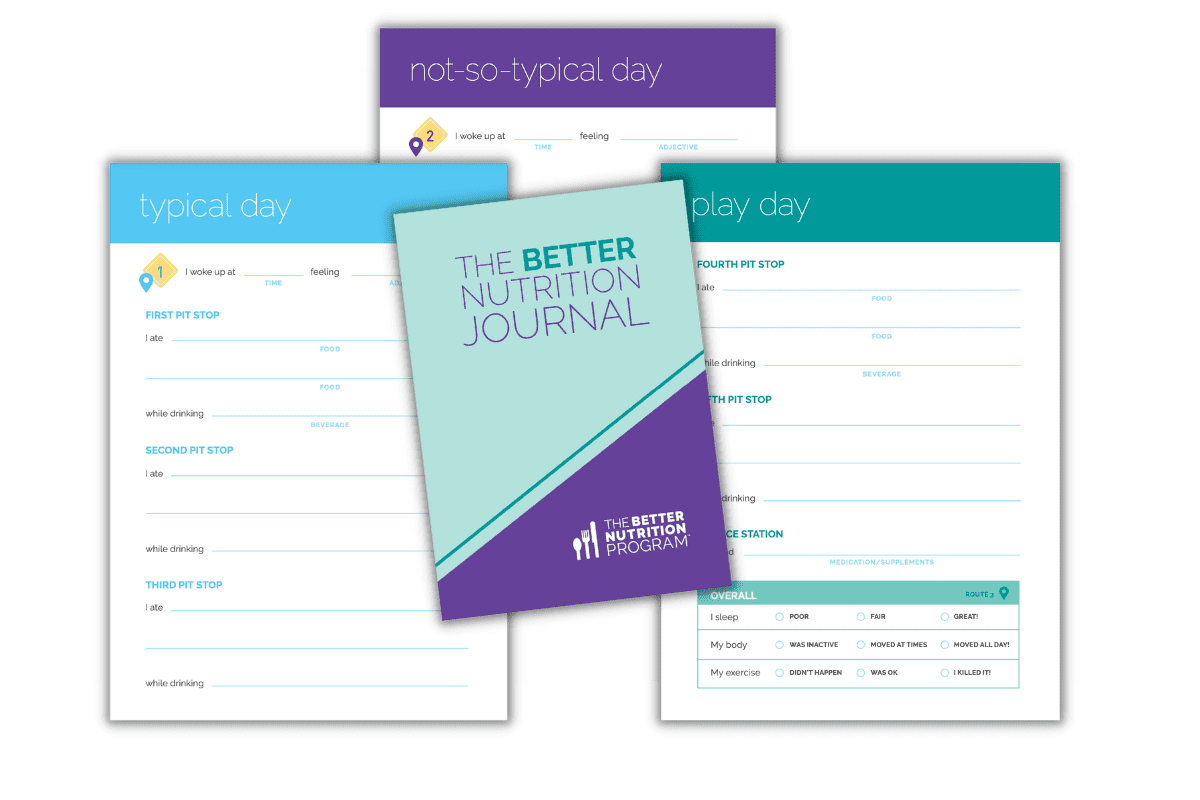
Continuous Glucose Monitors
The way to get a real understanding of what’s affecting your blood sugar is by looking at your blood sugar’s time in range. The way to do that is by wearing a Continuous Glucose Monitor (CGM) for 14 days. But to take away actionable insights, that must be paired with logging food, sleep, activity and more and having access to qualified clinicians to extract those actionable insights and empower you to make real progress. If you pop on the CGM and look at your results without clinical interpretation, you’ll be tempted to make narrowly focused changes such as eating less sugar or simple carbs and…wait…isn’t that where we started this conversation? Make sure that if you’re going to wear a CGM, you have the qualified support to make sense of the information and help you make an actionable plan.
If your practitioner doesn’t have a comprehensive CGM program in place, we can help. Our Continuous Glucose Monitor Program provides you with a BNP coach (backed by a highly qualified clinical team) as your guide, you’ll explore your blood sugar in detail: what different levels mean, what different choices can feel like, and how day-to-day decisions can help you avoid cravings, improve performance, and stay on the road to better health.
Is GLP-1 the Solution to High Blood Sugar?
If you’ve been paying attention to issues around blood sugar, you’ve probably read about GLP-1. GLP-1 agonists are a class of medications for people with Type 2 Diabetes. They mimic a hormone called GLP-1, which helps the pancreas produce insulin. GLP-1 agonists, like GLP-1 itself, stimulate the pancreas to produce more insulin after meals and better regulate blood glucose levels.
The thing is…medications typically don’t correct the underlying condition – they just address the symptoms. This is not to say that people with Type 2 Diabetes shouldn’t get these medications. But what if rather than just giving the medicine, we understood why the body isn’t producing enough GLP-1 in the first place and that solved the problem?
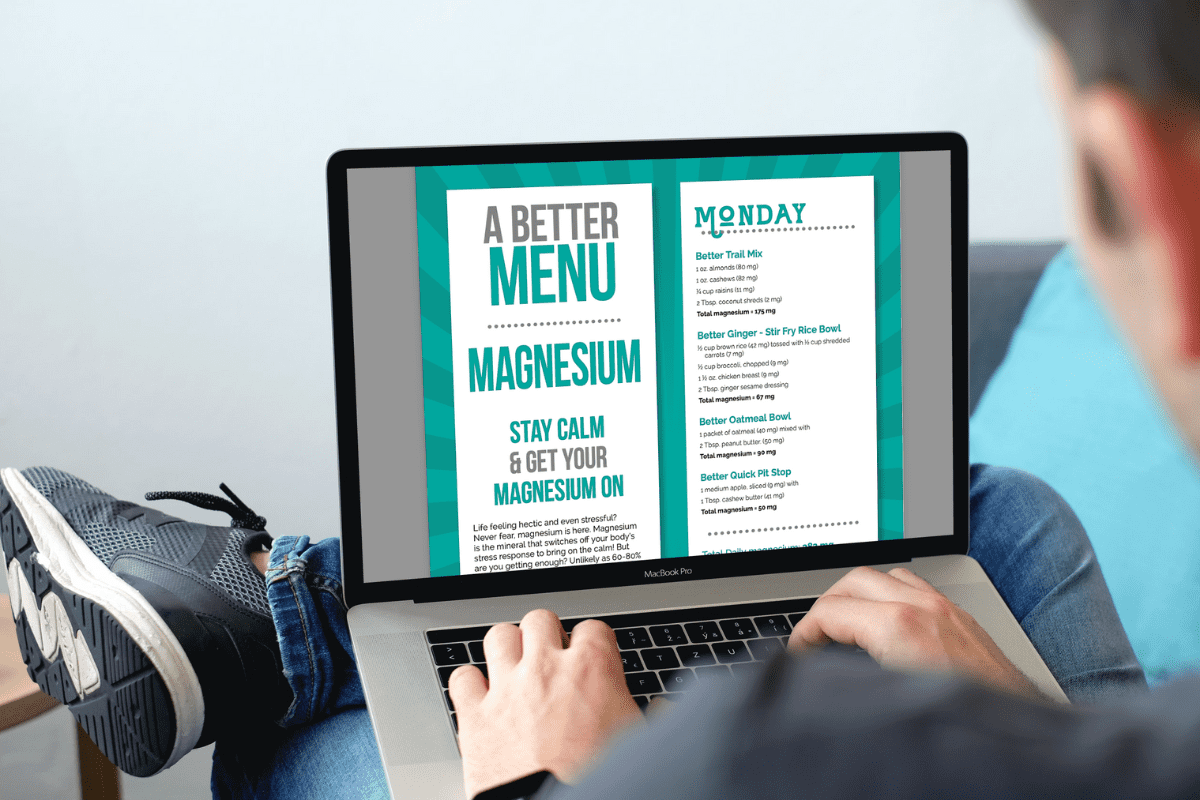
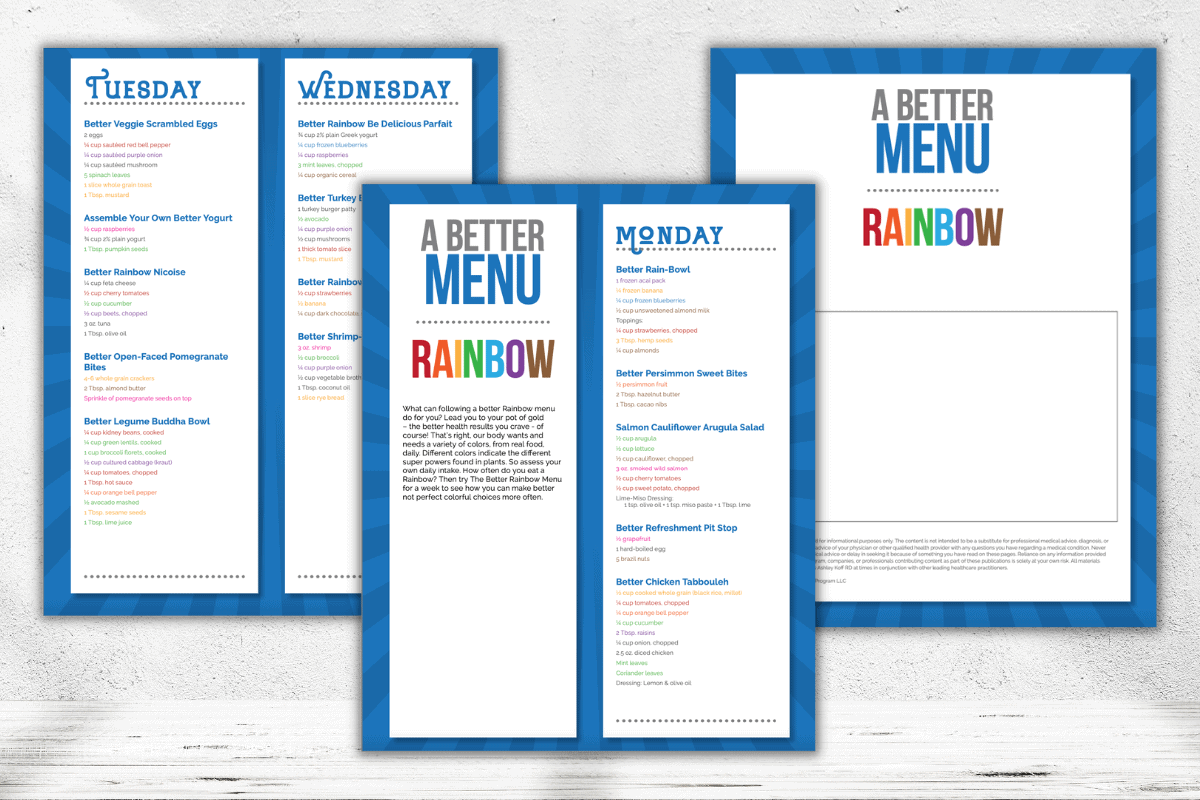
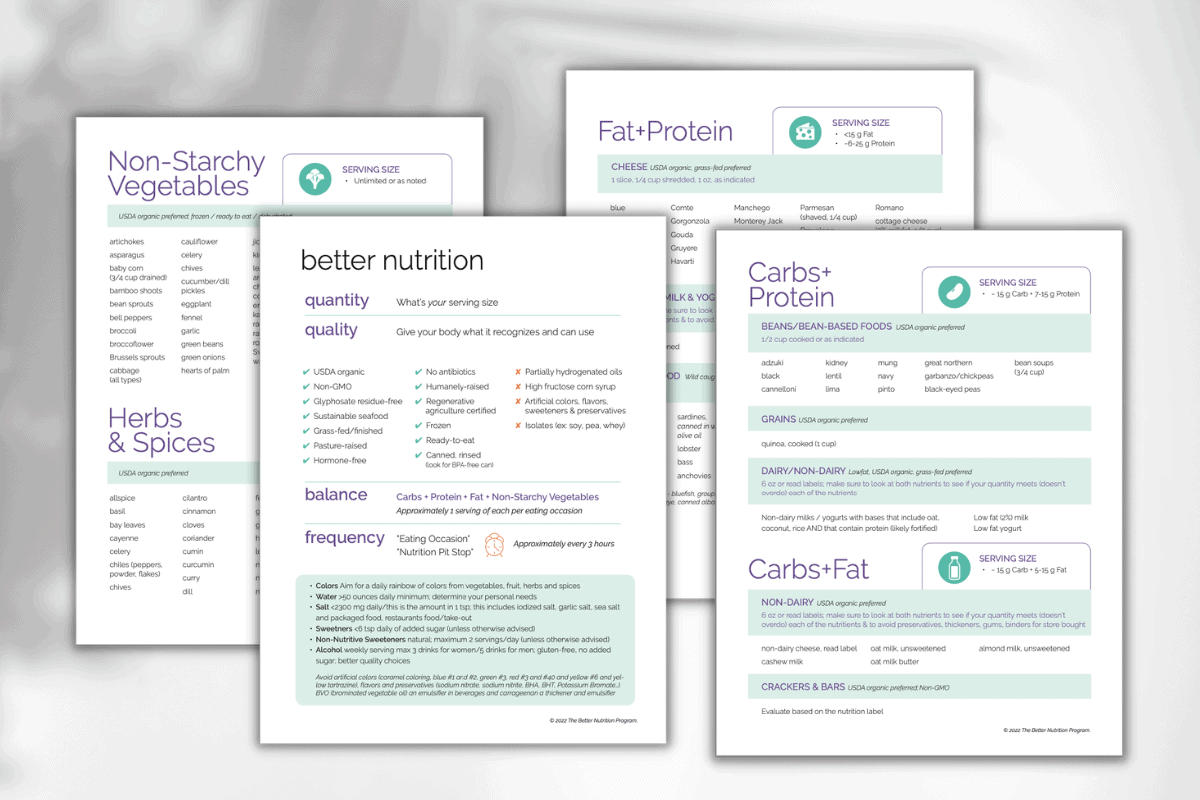
Several factors impact GLP-1 production and help improve overall health (which medications typically do not). Optimized GLP-1 production occurs with better nutrition — giving your body what it needs to run better while reducing what can irritate or overwhelm your system. This includes ensuring optimal levels of specific nutrients like potassium, magnesium, zinc, chromium, polyphenols and fibers, as well as specific strains of probiotics. It also requires reduction of chemical residues, environmental toxins, chemistry lab ingredients, and addressing elevated stress, digestive complaints, and poor sleep.
BNP’s Blood Sugar Optimizer program is the first program designed to improve GLP-1 production through nutrition and lifestyle choices, while also addressing underlying health issues. To learn more and to reserve a spot, head here.